Bile Duct Stricture
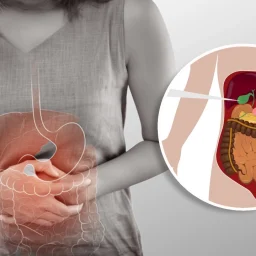
The bile ducts are a network of tubes that transport bile, a digestive fluid produced by the liver, from the liver to the gallbladder and from the gallbladder to the small intestine. Bile is necessary for the digestion of fats and for absorbing fat-soluble vitamins (A, D, E, and K).
Bile duct strictures refer to the narrowing or scarring of these bile ducts. This narrowing impedes the normal flow of bile and can lead to bile build-up in the liver, causing a range of issues such as jaundice, itching, pain, and even liver damage if left untreated.
2. Causes of Bile Duct Stricture
There are various causes of bile duct stricture, some of which are related to diseases, infections, or injuries. These causes can be broadly categorized as:
A. Inflammatory Conditions
One of the most common causes of bile duct stricture is inflammation that leads to scarring. This can occur in several conditions, including:

- Primary Sclerosing Cholangitis (PSC): PSC is a chronic disease characterized by inflammation and scarring of the bile ducts. Over time, this can lead to bile duct strictures and bile flow obstruction. PSC is often associated with other conditions, such as inflammatory bowel disease (IBD).
- Chronic Cholangitis: Inflammation of the bile ducts, often due to bacterial infections or other irritants, can lead to scarring and stricture formation. This can be seen in patients with recurrent episodes of cholangitis.
B. Injury or Surgery
- Post-Surgical Bile Duct Injury: Surgical procedures involving the gallbladder or liver, such as gallbladder removal (cholecystectomy) or liver transplants, can inadvertently damage the bile ducts. This injury can lead to bile duct strictures, either immediately after surgery or in the years that follow.
- Trauma or Injury: Any form of blunt or penetrating trauma to the abdomen that damages the bile ducts can cause strictures.
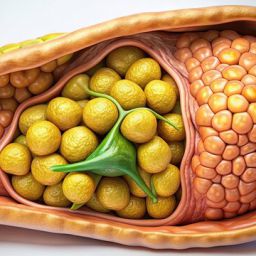
C. Gallstones
Gallstones are hardened deposits of bile that can form in the gallbladder. When these stones migrate into the bile ducts, they can cause blockages and lead to inflammation. This inflammation, especially if recurrent, can result in strictures over time. In some cases, large stones may physically damage the bile ducts, causing scarring and narrowing.
D. Cancer
Certain types of cancer can cause bile duct strictures by directly affecting the bile ducts or surrounding structures. These include:
- Bile Duct Cancer (Cholangiocarcinoma): This type of cancer originates in the cells of the bile ducts. As the tumor grows, it can constrict the bile ducts, leading to a stricture.
- Pancreatic Cancer: Tumors from the pancreas can invade or compress the bile ducts, leading to strictures and bile flow obstruction.
- Gallbladder Cancer: Similar to pancreatic cancer, gallbladder cancer can also cause bile duct strictures due to direct involvement of the bile ducts.
E. Autoimmune Conditions
Autoimmune diseases such as Autoimmune Hepatitis and Cystic Fibrosis can also be linked to bile duct stricture. In these conditions, the body’s immune system mistakenly attacks the bile ducts, leading to inflammation and narrowing of the ducts.
F. Infections
Infections, particularly chronic or recurrent infections of the bile ducts (like ascending cholangitis), can cause scarring and lead to strictures. These infections are often caused by bacteria that enter the bile ducts through the common bile duct or due to complications from gallstones.
3. Symptoms of Bile Duct Stricture
The symptoms of bile duct stricture can vary depending on the severity of the narrowing and the underlying cause. Common symptoms include:

- Jaundice: One of the most common signs of bile duct stricture is jaundice, which causes yellowing of the skin and eyes. This occurs when bile builds up in the liver and is unable to flow into the small intestine.
- Abdominal Pain: Patients may experience pain in the upper right side of the abdomen, which can range from dull to sharp.
- Fatigue: Chronic obstruction of bile flow can cause fatigue, as the body struggles to digest fats and absorb essential nutrients.
- Itching (Pruritus): The build-up of bile salts in the bloodstream can lead to intense itching, particularly on the palms of the hands and the soles of the feet.
- Dark Urine: Increased levels of bilirubin in the bloodstream can result in dark, tea-colored urine.
- Nausea and Vomiting: As bile flow is obstructed, patients may also experience nausea and vomiting, particularly after eating fatty foods.
- Digestive Issues: Bile duct strictures can cause difficulty in digesting fats, leading to diarrhea, bloating, and unintentional weight loss.
4. Diagnosis of Bile Duct Stricture
Early diagnosis of bile duct stricture is essential to prevent further complications, including liver damage. The following diagnostic tests may be used to identify the condition:
A. Imaging Tests
- Ultrasound: This non-invasive imaging test is commonly used as a first step in diagnosing bile duct strictures. It can detect bile duct enlargement, gallstones, and signs of obstruction.
- Magnetic Resonance Cholangiopancreatography (MRCP): MRCP is a type of MRI scan that provides detailed images of the bile ducts and can help diagnose strictures and blockages.
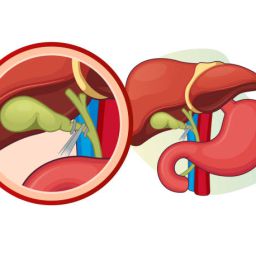
- Endoscopic Retrograde Cholangiopancreatography (ERCP): ERCP combines endoscopy and fluoroscopy to visualize the bile ducts directly. It allows the doctor not only to diagnose strictures but also to perform interventions, such as stent placement or stone removal.
B. Blood Tests
Blood tests can help assess liver function, which may be affected by bile duct obstruction. Elevated liver enzymes (AST, ALT) and bilirubin levels are common in individuals with bile duct strictures.
C. Biopsy
In cases where cancer or other serious conditions are suspected, a biopsy may be performed to collect tissue samples from the bile ducts for further analysis.
5. Treatment of Bile Duct Stricture
Treatment for bile duct stricture depends on the underlying cause, severity of the stricture, and overall health of the patient. Options may include:
A. Endoscopic Procedures
- Stent Placement: In cases of benign bile duct strictures, a doctor may use an endoscope to place a stent (a small tube) in the bile duct to keep it open and allow bile to flow normally.
- Balloon Dilation: This procedure involves the insertion of a balloon into the stricture to widen the narrowed bile duct.
B. Surgery
- Biliary Bypass Surgery: In severe cases, where the stricture cannot be treated with endoscopic procedures, surgery may be required to bypass the obstructed bile duct.
- Bile Duct Reconstruction: This type of surgery is necessary if there has been significant damage to the bile ducts. The surgeon may reconstruct the bile duct to restore bile flow.
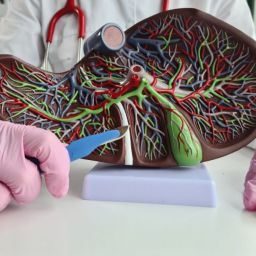
C. Liver Transplantation
In cases of chronic bile duct strictures that lead to irreversible liver damage or cirrhosis, a liver transplant may be considered.
D. Medication
In cases where inflammation is the cause of the stricture (such as in PSC or chronic cholangitis), medications like corticosteroids or immunosuppressive drugs may be used to reduce inflammation and manage symptoms.
6. Prevention of Bile Duct Stricture
While not all cases of bile duct stricture can be prevented, certain measures can reduce the risk, such as:
- Prompt Treatment of Gallstones: Early intervention for gallstones can help prevent blockages and inflammation that may lead to strictures.
- Careful Surgical Techniques: Surgeons should exercise caution when performing surgeries on the gallbladder or liver to avoid damage to the bile ducts.
- Managing Underlying Conditions: Proper management of diseases such as PSC, chronic cholangitis, and autoimmune conditions can reduce the risk of developing bile duct strictures.
Bile duct stricture is a serious condition that can lead to significant health issues if not diagnosed and treated promptly. It can result from a variety of causes, including inflammation, injury, infections, cancer, and autoimmune conditions. Early diagnosis through imaging tests, blood work, and sometimes biopsies is critical for effective treatment. Treatment options range from endoscopic interventions, such as stent placement and balloon dilation, to surgery and liver transplantation in severe cases. By understanding the causes and symptoms of bile duct stricture, patients can work with healthcare providers to develop a treatment plan and improve their quality of life.