As we age, various aspects of our health undergo changes, and one of the areas that require particular attention is colon health. The colon, also known as the large intestine, plays a critical role in digestion, water absorption, and overall gut function. Aging brings with it a series of changes in colon function, which can impact bowel movements, increase the risk of diseases, and affect the quality of life. Understanding these changes is essential for promoting colon health in older adults and preventing common conditions associated with aging.
1. The Aging Process and Its Impact on Colon Function
As we age, our bodies undergo several changes that affect the gastrointestinal (GI) system. These changes, including slower digestion, reduced motility, and shifts in microbiota composition, can all have an impact on the colon. Let’s explore these physiological changes in greater detail:
Slower Digestion and Motility
- Decreased Peristalsis: Peristalsis is the wave-like contraction of muscles that moves food through the digestive tract. As we age, these contractions tend to slow down, leading to longer transit times in the colon. This can result in constipation, a common issue in older adults.
- Reduced Muscle Tone: The muscles of the colon can weaken with age, further contributing to reduced motility. This makes it more difficult for the colon to push stool through the intestine efficiently.
Altered Gut Microbiota
- Dysbiosis: As people age, there tends to be an imbalance in the gut microbiota, known as dysbiosis. The diversity of beneficial bacteria in the colon decreases, and harmful bacteria may proliferate. This imbalance can contribute to digestive issues such as constipation, diarrhea, and bloating.
- Immune Function Decline: A healthy microbiota helps support the immune system by producing short-chain fatty acids (SCFAs) and other metabolites that regulate immune responses. Aging reduces the capacity of the immune system to respond to harmful pathogens and inflammation, making the colon more susceptible to infections and diseases.
2. Common Digestive Issues in Older Adults
As the colon ages, several common digestive issues become more prevalent. Let’s discuss these conditions and their relationship to aging:
Constipation
- Increased Risk with Age: Constipation becomes more common with age, affecting a significant portion of older adults. This can be due to slower motility, reduced physical activity, and dietary changes that may be less fiber-rich. Medications that older adults may take for other conditions can also exacerbate constipation.
Diverticular Disease
- Diverticulosis and Diverticulitis: Diverticular disease is a common condition that affects the colon as we age. Diverticulosis refers to the formation of small pouches (diverticula) in the wall of the colon. These pouches can become inflamed or infected, leading to diverticulitis. This condition becomes more common in individuals over the age of 40 and can cause abdominal pain, bloating, and changes in bowel habits.
Irritable Bowel Syndrome (IBS)
- Impact of Aging on IBS: While IBS is often diagnosed in younger individuals, the symptoms of IBS—such as abdominal pain, bloating, and irregular bowel movements—can persist into older age. In fact, the aging process can make IBS symptoms more difficult to manage, due to changes in diet, medication use, and other underlying health conditions.
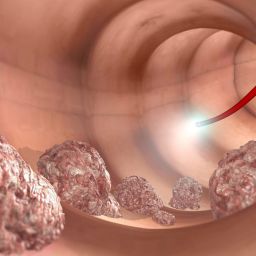
Colorectal Cancer
- Increased Risk with Age: The risk of colorectal cancer increases with age, particularly after the age of 50. Genetic factors, a history of polyps, a sedentary lifestyle, and a poor diet can all contribute to the increased risk of developing colon cancer as one ages.
- Importance of Screening: Early detection through regular screening, such as colonoscopies, can help identify colorectal cancer at its early stages and improve the chances of successful treatment. For older adults, it is essential to continue regular screening even as they age, particularly if they have a family history of colon cancer.
3. How Lifestyle Factors Influence Colon Health in Older Adults
While aging brings physiological changes to the colon, certain lifestyle factors can significantly influence colon health in older adults. Let’s explore some of these factors:
Dietary Factors
- Fiber Intake: One of the most important aspects of maintaining colon health as we age is ensuring adequate fiber intake. A high-fiber diet promotes regular bowel movements and supports a healthy microbiome. Fiber-rich foods such as fruits, vegetables, whole grains, and legumes are essential for preventing constipation and other digestive issues.
- Limit Processed Foods: As we age, it is crucial to limit the consumption of processed foods, red meat, and foods high in saturated fats. These types of foods can increase the risk of colon cancer, diverticulosis, and other digestive conditions.
- Hydration: Dehydration is a common problem in older adults, and it can significantly impact colon health. Ensuring proper hydration is essential for maintaining regular bowel movements and preventing constipation.
Physical Activity
- Exercise and Colon Health: Regular physical activity is critical for promoting healthy digestion. Exercise helps to stimulate peristalsis, reduce inflammation, and support overall gut health. Older adults should engage in regular exercise, such as walking, swimming, or yoga, to promote healthy colon function and reduce the risk of digestive problems.
Medication Use
- Medications and Digestive Health: Many older adults take medications for various health conditions, and some of these can negatively affect colon health. For instance, pain medications, antidepressants, and antacids can contribute to constipation or alter gut motility. It is important for older adults to discuss any medication concerns with their healthcare provider and explore alternatives if necessary.
4. Strategies to Maintain Colon Health in Older Adults
Maintaining colon health as we age is achievable with proper care and lifestyle modifications. Below are strategies that older adults can adopt to support a healthy colon:

1. Regular Screenings
- Colonoscopies and Early Detection: Regular screenings for colorectal cancer are essential for detecting early-stage cancer and polyps, which may later develop into cancer. For those over 50 or those at higher risk, colonoscopies are highly recommended.
2. Eating a Balanced, Fiber-Rich Diet
- Incorporating More Fiber: A diet rich in fiber is essential for promoting regular bowel movements, reducing the risk of constipation, and maintaining a healthy microbiome. Older adults should aim for a daily intake of 25-30 grams of fiber from whole grains, fruits, and vegetables.
- Probiotics and Gut Health: Incorporating probiotics or fermented foods into the diet can help restore balance to the gut microbiota and improve colon health.
3. Staying Active
- Regular Exercise: Engaging in regular physical activity, even light exercise such as walking, can help stimulate digestion, improve motility, and prevent constipation.
4. Hydration
- Drinking Plenty of Water: Maintaining hydration is essential for healthy digestion and preventing constipation. Older adults should ensure they are drinking adequate amounts of water throughout the day.
5. Managing Stress
- Stress and Gut Health: Chronic stress can negatively impact gut function. Practicing stress-reducing activities such as meditation, deep breathing exercises, or yoga can help improve overall colon health.
Taking Action for Healthy Colon Health in Older Age
The aging process inevitably brings changes to colon health, but with proper care, these changes can be managed and even prevented. A balanced diet, regular physical activity, regular screenings, and attention to hydration and stress management can significantly improve colon health in older adults. By adopting these strategies, older individuals can maintain a healthy colon, prevent common digestive issues, and reduce the risk of more severe conditions such as colorectal cancer. Taking a proactive approach to colon health can lead to better digestive function, a higher quality of life, and improved overall well-being as we age.