The Colon and Its Role in Gut Health
The colon is the last part of the digestive tract, responsible for absorbing water, electrolytes, and certain nutrients from the indigestible remnants of food. In addition to water absorption, the colon serves as a habitat for trillions of bacteria that make up the gut microbiota, which has significant implications for digestion, immune system function, and even mental health.
Colon health is impacted by various factors, including the balance of microbiota, the functionality of receptors, and hormonal signaling within the body. Disruptions to any of these systems can lead to a variety of digestive disorders and systemic health issues.
1. G-Protein Coupled Receptors (GPCRs)
GPCRs are the largest family of receptors involved in cellular signaling in the colon. They are responsible for mediating responses to neurotransmitters, hormones, and other signaling molecules. GPCRs in the colon regulate functions such as motility, secretion, and absorption.

- Enteric Nervous System (ENS): The ENS is often referred to as the “second brain” due to its vast network of neurons. GPCRs in the ENS help coordinate the contractions of smooth muscles in the colon, influencing peristalsis (the wave-like motion that moves food through the gut).
- Serotonin Receptors: Serotonin, a neurotransmitter primarily known for its role in mood regulation, is also crucial for regulating gut motility. Serotonin receptors (5-HT receptors) in the colon influence peristalsis and can affect the frequency of bowel movements. Disruptions in serotonin signaling are associated with conditions such as irritable bowel syndrome (IBS).
2. Toll-Like Receptors (TLRs)
Toll-like receptors are a class of proteins involved in the innate immune system. These receptors are located on the surface of cells in the colon and are responsible for detecting pathogens and signaling the immune response. TLRs are particularly important in maintaining gut health by detecting harmful microorganisms in the gut and triggering appropriate immune reactions.
- TLR4: This receptor plays a key role in detecting bacterial lipopolysaccharides (LPS), a component of the cell walls of certain bacteria. Activation of TLR4 can trigger inflammation, which is an important defense mechanism. However, chronic activation of TLR4 can contribute to inflammatory bowel diseases (IBD) such as Crohn’s disease and ulcerative colitis.
3. Cannabinoid Receptors (CB1 and CB2)
The endocannabinoid system plays a role in regulating a variety of functions within the gut, including motility, pain sensation, and immune responses. Cannabinoid receptors, specifically CB1 and CB2, are found in the colon and modulate gut function.
- CB1 Receptors: These receptors are primarily involved in regulating intestinal motility and secretion. They are often targeted in the treatment of IBS, as modulation of CB1 receptors can help alleviate symptoms such as diarrhea and constipation.
- CB2 Receptors: CB2 receptors are involved in the modulation of immune responses in the colon. They help reduce inflammation and play a protective role in conditions such as IBD and colorectal cancer.
The Impact of Gut Microbiota on Colon Health
Gut microbiota, the trillions of microorganisms residing in the colon, plays a crucial role in maintaining gut health. These bacteria help digest food, produce vitamins, and regulate the immune system. The balance of beneficial and harmful bacteria within the gut is essential for preventing disease.
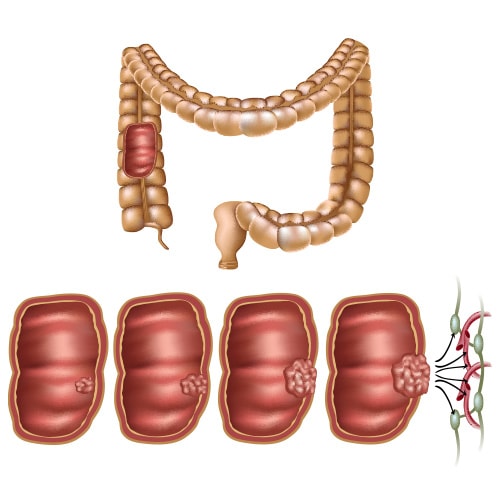
1. Dysbiosis and Colon Disease
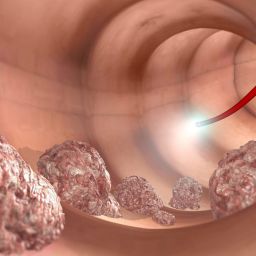
When the balance of gut microbiota is disrupted, a condition known as dysbiosis occurs. Dysbiosis can lead to inflammation, compromised gut barrier function, and an increased risk of diseases such as IBD, IBS, and colon cancer.
- Inflammatory Bowel Disease (IBD): Studies have shown that individuals with IBD have an altered gut microbiome, with an overgrowth of harmful bacteria and a reduction in beneficial microbes. The inflammation in IBD is thought to result from an exaggerated immune response to this altered microbiota.
- Colon Cancer: Dysbiosis has also been linked to an increased risk of colon cancer. Certain bacteria can produce carcinogenic compounds, while others help regulate the immune response to cancerous cells. The gut microbiome may influence colon cancer development by modulating inflammation and promoting the production of protective immune cells.
2. Probiotics and Gut Health
Probiotics are live beneficial bacteria that can help restore the balance of gut microbiota. These bacteria may promote the growth of healthy microbes and suppress the growth of harmful bacteria. Probiotics have been studied for their potential benefits in treating conditions such as IBS, IBD, and even colon cancer.
- Regulating Immune Function: Probiotics can help modulate the immune system, reducing inflammation and promoting the production of regulatory T-cells that protect against autoimmune diseases.
- Improving Gut Barrier Function: Probiotics can also strengthen the gut barrier, preventing harmful substances from crossing into the bloodstream and reducing the risk of systemic inflammation.
Hormonal Regulation of Gut Health
Hormones play a significant role in regulating gut function, including digestion, motility, and the immune response.
1. Gut Hormones and Motility
The colon is regulated by a variety of gut hormones, including gastrin, cholecystokinin (CCK), secretin, and ghrelin. These hormones influence motility, secretion, and appetite.
- Ghrelin: Known as the “hunger hormone,” ghrelin is produced in the stomach and colon. It stimulates appetite and plays a role in regulating the frequency of bowel movements.
- Cholecystokinin (CCK): This hormone stimulates bile secretion and promotes digestion. It also regulates the motility of the small intestine and colon, helping to coordinate the digestive process.
2. Inflammatory Cytokines
Inflammatory cytokines, such as tumor necrosis factor (TNF) and interleukins (IL-6, IL-1β), are important regulators of immune function in the colon. Chronic inflammation, driven by the overproduction of these cytokines, is a hallmark of conditions such as IBD and colon cancer.
- TNF-α: This cytokine plays a central role in the development of inflammatory conditions and is a target for biologic therapies used in treating IBD.
Lifestyle and Diet: Influencing Gut Health and Colon Receptors
External factors such as diet, stress, and exercise can have a significant impact on colon receptors and gut health. These factors can either support or disrupt the function of receptors, the microbiota, and the immune system.
1. Dietary Fiber and Colon Health
A diet rich in fiber is essential for maintaining healthy colon function. Fiber promotes healthy bowel movements, reduces constipation, and helps maintain the balance of gut microbiota. It is also known to affect the activity of certain receptors, such as serotonin and GPCRs, which regulate motility and digestion.
- Prebiotics: Certain fibers act as prebiotics, promoting the growth of beneficial gut bacteria. Foods such as garlic, onions, and bananas are rich in prebiotics that support gut health.
2. Probiotics and Fermented Foods
Fermented foods such as yogurt, kefir, and sauerkraut are rich in probiotics that can support gut health by promoting the growth of beneficial bacteria and enhancing the function of gut receptors.
The Gut-Brain Connection: How the Brain Regulates Colon Health
The gut and the brain are closely connected through the enteric nervous system (ENS) and the vagus nerve. This complex communication system, often referred to as the “gut-brain axis,” influences gut motility, secretion, and immune responses, as well as emotional and psychological well-being.
1. Stress and Its Impact on Gut Health
Stress has a direct impact on the gut, influencing the function of gut receptors and the overall balance of the microbiota. Chronic stress can lead to changes in gut motility, an imbalance in gut bacteria, and an increase in intestinal permeability (commonly referred to as “leaky gut”). These disruptions can contribute to conditions like IBS, IBD, and even depression and anxiety.
- Corticotropin-Releasing Hormone (CRH): Under stress, the body releases CRH, a hormone that impacts the ENS and affects colon motility. Increased CRH levels can exacerbate gut issues by altering the gut’s ability to absorb nutrients and maintain proper function.
- The Role of the Vagus Nerve: The vagus nerve helps regulate gut functions such as motility and secretion, and it plays a central role in the gut-brain axis. By modulating the vagus nerve, it is possible to influence digestive processes and even alleviate some symptoms of stress-related gut disorders.
Understanding the Colon’s Role in Gut Health
The colon plays a central role in maintaining digestive health, regulating the microbiota, and supporting the immune system. A variety of receptors within the colon, including GPCRs, serotonin receptors, and cannabinoid receptors, help regulate colon motility, immune responses, and gut barrier integrity. Additionally, hormonal signaling and the gut-brain axis play key roles in maintaining a healthy gut.
Understanding how these receptors and body factors regulate colon health can lead to better preventative measures, early detection of diseases, and more effective treatments for colon-related conditions. By making informed choices about diet, exercise, and stress management, individuals can significantly improve their gut health and reduce the risk of conditions such as IBS, IBD, and colon cancer.