1. Traditional Surgery: Open Surgery
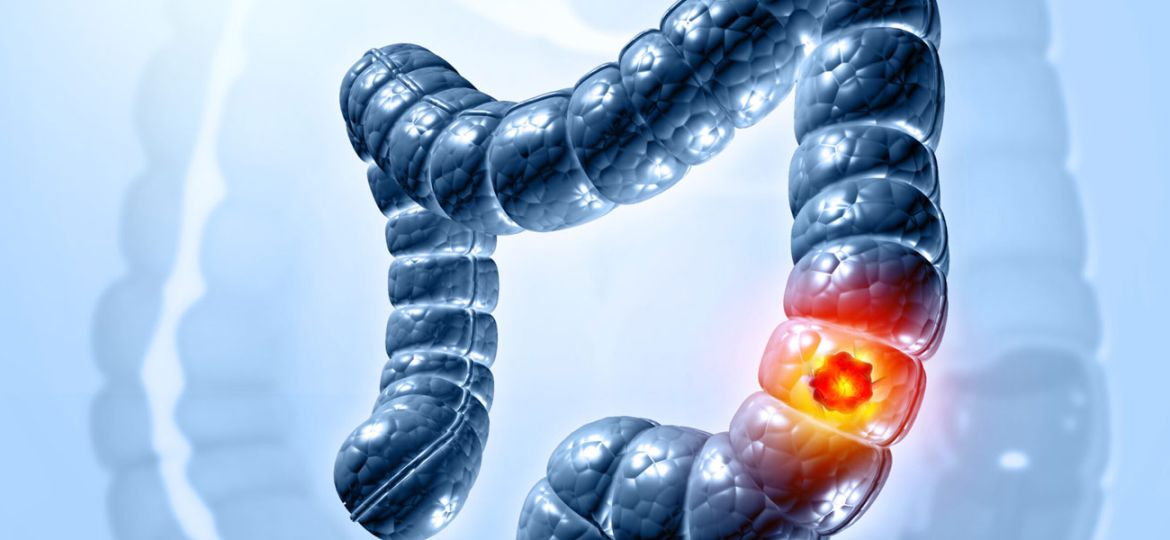
Open surgery is one of the most commonly used methods for the treatment of colorectal cancer. It involves making a large incision in the abdomen to access the affected part of the colon or rectum. The goal is to remove the tumor and surrounding tissue to ensure that no cancerous cells remain.
Procedure
In open surgery, the surgeon makes a single, long incision in the abdominal wall to reach the colon or rectum. The affected portion of the colon is then removed, along with nearby lymph nodes to check for cancer spread. The surgeon may need to create a temporary or permanent colostomy, depending on the extent of the surgery.
Advantages and Disadvantages
The primary advantage of open surgery is its ability to provide a clear view of the area and to remove large tumors. However, the procedure is invasive, leading to a longer recovery time, increased pain, and a higher risk of complications like infections and blood loss.

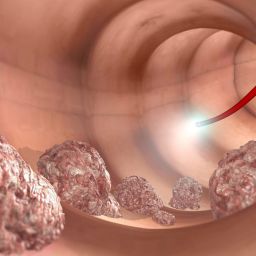
2. Minimally Invasive Surgery: Laparoscopic Surgery
Laparoscopic surgery, also known as minimally invasive surgery (MIS), is an advanced surgical technique that uses small incisions and a camera to guide the surgeon in removing the cancerous tissue. This method has gained popularity due to its advantages in recovery time, reduced pain, and fewer complications.
Procedure
During laparoscopic surgery, the surgeon makes several small incisions in the abdomen. A long, thin tube with a camera (laparoscope) is inserted through one incision, providing the surgeon with a magnified view of the inside of the abdomen. Specialized instruments are then used to remove the tumor and nearby tissue. In some cases, the surgeon may convert the laparoscopic surgery to an open procedure if complications arise.
Advantages and Disadvantages
The major benefits of laparoscopic surgery include shorter hospital stays, less postoperative pain, and quicker recovery times. Patients are typically able to return to normal activities within a few weeks. However, laparoscopic surgery requires a high level of skill and experience, and not all patients are candidates for this type of surgery, especially those with large or complex tumors.
3. Robotic Surgery
Robotic surgery is an advancement of laparoscopic surgery that utilizes robotic systems to assist in the procedure. The most common robotic system used for colorectal cancer surgery is the da Vinci Surgical System, which allows surgeons to operate with greater precision.
Procedure
The surgeon controls the robotic arms while sitting at a console, using hand and foot controls to manipulate the instruments and perform the surgery. The robot provides enhanced 3D visualization, greater dexterity, and improved precision in tissue manipulation, which is particularly beneficial in complex or delicate procedures.
Advantages and Disadvantages
Robotic surgery offers several benefits, such as improved precision, less bleeding, and faster recovery. The minimally invasive nature of the surgery reduces trauma to the body and minimizes scarring. However, it is more expensive than traditional surgery and may not be available in all medical centers. It also requires specialized training for surgeons.
4. Sphincter-Saving Surgery
In cases where colorectal cancer is located in the rectum, surgeons aim to preserve the anus and sphincter muscles to allow for normal bowel function after surgery. Sphincter-saving surgery is often possible in early-stage rectal cancers but may not be feasible in more advanced cases.
Procedure
If the tumor is located in the lower part of the rectum but has not spread too far, the surgeon can remove the tumor while preserving the anal sphincter. This procedure is also known as low anterior resection (LAR). It involves removing the tumor along with a portion of the surrounding healthy tissue, while ensuring that the sphincter muscles remain intact.
Advantages and Disadvantages
The benefit of sphincter-saving surgery is that it allows patients to avoid the need for a permanent colostomy, thereby maintaining bowel control. However, this procedure is complex and not always possible, particularly if the cancer is too close to the anus. In such cases, an abdominoperineal resection (APR) may be necessary, which results in the removal of the anus and the creation of a permanent colostomy.
5. Colostomy and Ileostomy Surgery
In some cases of colorectal cancer, the colon or rectum may need to be permanently or temporarily bypassed due to extensive removal of tissue. Colostomy and ileostomy surgeries are procedures that divert the bowel’s waste products into a bag or pouch outside the body.

Procedure
A colostomy involves creating an opening (stoma) in the abdomen, where the colon is connected to the surface of the skin. Waste material is then collected in a bag worn on the outside of the body. In an ileostomy, the ileum (the last part of the small intestine) is diverted to the stoma, bypassing the colon entirely.
Advantages and Disadvantages
The main advantage of a colostomy or ileostomy is that it can be life-saving when the colon or rectum must be removed. However, it can be emotionally and physically challenging for patients, as they must adapt to living with a stoma and managing the pouch. In some cases, these procedures are temporary, with the possibility of reversal after the area heals.
6. Preoperative and Postoperative Considerations
Before undergoing surgery for colorectal cancer, patients are often evaluated for their overall health, including the assessment of their cardiovascular, pulmonary, and renal systems. Preoperative measures may also include bowel preparation, which involves clearing the colon to reduce the risk of infection.
Postoperative Care
After surgery, patients typically spend several days in the hospital to monitor for complications such as infections, bleeding, or bowel obstruction. Pain management, physical therapy, and dietary adjustments are crucial for a smooth recovery. In some cases, chemotherapy or radiation therapy may follow surgery to ensure that any remaining cancer cells are eradicated.
7. Recovery and Long-Term Outlook
Recovery from colorectal cancer surgery varies depending on the type of surgery performed, the patient’s overall health, and the stage of cancer. Generally, patients can expect a hospital stay of several days to a week, with a gradual return to normal activities over a period of weeks to months.
Post-Surgery Lifestyle Changes
Post-surgery, patients may need to make lifestyle changes, including dietary adjustments, exercise, and possibly colostomy care. Regular follow-up appointments are essential to monitor for recurrence, and some patients may require additional treatments such as chemotherapy or radiation therapy.
Surgical treatment is a vital aspect of managing colorectal cancer, with several methods available depending on the tumor’s size, location, and stage. While traditional open surgery remains a common approach, laparoscopic and robotic-assisted surgeries have revolutionized the field, providing patients with less invasive options and faster recovery times. Sphincter-preserving surgeries and ostomy procedures further demonstrate the progress in colorectal cancer care, aiming to improve the quality of life for patients. Through careful preoperative assessment, surgical precision, and postoperative care, the outlook for patients with colorectal cancer has significantly improved, making surgery an essential tool in the fight against this disease.