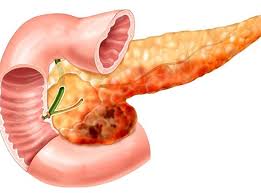
Reasons for Recurrence of Pancreatitis
Several factors contribute to the recurrence of pancreatitis, ranging from lifestyle choices to underlying medical conditions. In both acute and chronic pancreatitis, the recurrence is often linked to unresolved causes or risk factors that lead to repeated inflammation of the pancreas. Below are the most common reasons why pancreatitis may recur:
1. Continued Alcohol Consumption
One of the primary causes of recurrent pancreatitis, particularly chronic pancreatitis, is alcohol consumption. Alcohol is a known irritant to the pancreas, and excessive drinking can lead to repeated episodes of inflammation. Alcohol-induced pancreatitis is a significant risk factor for chronic pancreatitis, and even after a patient has recovered from an initial episode, continued drinking can trigger another episode of inflammation.
For individuals with chronic pancreatitis, alcohol consumption is particularly problematic because it can exacerbate the existing damage to the pancreas and accelerate the progression of the disease. Even moderate drinking can lead to a relapse, making alcohol cessation a critical part of managing and preventing the recurrence of pancreatitis.
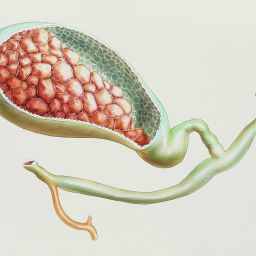
2. Gallstones and Biliary Obstruction

Gallstones are another leading cause of pancreatitis, particularly acute pancreatitis. Gallstones can obstruct the bile duct or the pancreatic duct, leading to inflammation of the pancreas. When the bile duct is blocked, bile and digestive enzymes back up into the pancreas, causing it to become inflamed. If the underlying cause of the blockage, such as gallstones, is not treated or managed, pancreatitis may recur.
In many cases, individuals who experience pancreatitis due to gallstones may undergo a procedure to remove the gallbladder (cholecystectomy) to prevent further episodes. However, if the stones are not fully removed or if new stones form after surgery, pancreatitis may return.
3. High Triglyceride Levels
Elevated triglycerides in the blood can trigger pancreatitis, especially when triglyceride levels exceed 1,000 mg/dL. Hypertriglyceridemia is a known cause of both acute and recurrent pancreatitis. High triglyceride levels may occur due to genetic predisposition, obesity, diabetes, excessive alcohol consumption, or poor diet. In many cases, individuals with hypertriglyceridemia may experience repeated episodes of pancreatitis unless the underlying cause of the elevated triglycerides is addressed.
Managing triglyceride levels through lifestyle changes, such as a low-fat diet, regular exercise, and medication, is essential in reducing the risk of recurrence. However, if triglyceride levels are not adequately controlled, the risk of recurrent pancreatitis remains high.
4. Pancreatic Duct Obstruction
Obstruction of the pancreatic duct can lead to recurrent episodes of pancreatitis. The pancreatic duct is responsible for transporting digestive enzymes from the pancreas to the small intestine. Any obstruction of this duct, whether due to gallstones, tumors, or scarring from previous episodes of pancreatitis, can result in a backup of enzymes into the pancreas, leading to inflammation.
Pancreatic duct obstructions may require surgical intervention to remove the blockage or bypass the obstructed area. If the obstruction is not fully resolved or if scarring continues to progress, pancreatitis may recur.
5. Genetic Factors
Some individuals have a genetic predisposition to developing pancreatitis, and this can lead to recurrent episodes, especially in the case of hereditary pancreatitis. Hereditary pancreatitis is a rare genetic condition that causes individuals to have a higher risk of developing pancreatitis at an earlier age. The most common genetic mutation associated with hereditary pancreatitis is a mutation in the PRSS1 gene, which causes abnormal production of digestive enzymes.
In hereditary pancreatitis, individuals are at a significantly higher risk of experiencing repeated episodes of pancreatitis, often starting in childhood or early adulthood. Genetic counseling and regular monitoring are essential for individuals with a family history of hereditary pancreatitis to manage the condition and prevent recurrence.
6. Autoimmune Pancreatitis
Autoimmune pancreatitis is a type of pancreatitis in which the body’s immune system attacks the pancreas, leading to inflammation. It is a rare form of pancreatitis that can cause recurrent episodes. Autoimmune pancreatitis is often associated with other autoimmune conditions, such as IgG4-related disease or primary sclerosing cholangitis.
The recurrence of autoimmune pancreatitis is typically linked to the flare-ups of the autoimmune response. Treatment for autoimmune pancreatitis often involves the use of corticosteroids or immunosuppressive medications to control the immune system’s activity. However, if the condition is not adequately managed, inflammation can return, leading to recurrent pancreatitis.
7. Smoking
Smoking is another significant risk factor for the recurrence of pancreatitis, particularly in individuals who already have chronic pancreatitis. Smoking can contribute to pancreatic inflammation and exacerbate the damage caused by previous episodes. Research has shown that individuals with chronic pancreatitis who smoke are more likely to experience more frequent and severe flare-ups of the disease. Smoking can also accelerate the progression of chronic pancreatitis, increasing the risk of complications such as pancreatic cancer.
8. Poor Dietary Habits
A diet high in fatty foods, processed sugars, and low in fiber can contribute to the recurrence of pancreatitis, especially in individuals who are already at risk due to other factors. High-fat diets, in particular, can increase triglyceride levels, triggering acute pancreatitis or worsening chronic pancreatitis. Additionally, an unhealthy diet can lead to obesity and metabolic syndrome, which are also linked to recurrent pancreatitis.
To prevent recurrence, individuals with pancreatitis are advised to follow a low-fat, balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Proper hydration and avoiding excessive alcohol intake are also important dietary considerations.
9. Medication Side Effects
Certain medications, such as diuretics, antibiotics, and statins, can trigger pancreatitis as a side effect. While this is relatively rare, it can lead to recurrent episodes of inflammation in susceptible individuals. If a medication is found to be the cause of pancreatitis, the healthcare provider may adjust the treatment plan to avoid further episodes.
Managing and Preventing Recurrent Pancreatitis
Preventing recurrent pancreatitis requires a multifaceted approach, targeting the underlying causes and risk factors that contribute to inflammation. Below are some strategies to help manage and prevent the recurrence of pancreatitis:

1. Lifestyle Changes
The most effective way to prevent recurrent pancreatitis is by making lifestyle changes that address the underlying causes. This includes:
- Abstinence from alcohol: For individuals with alcohol-induced pancreatitis, complete abstinence is necessary to prevent further episodes.
- Dietary modifications: Following a low-fat, nutrient-rich diet can help reduce triglyceride levels and prevent further episodes of pancreatitis.
- Weight management: Maintaining a healthy weight through regular exercise and a balanced diet is crucial in managing triglyceride levels and reducing the risk of recurrent pancreatitis.
2. Medical Management
For individuals with specific risk factors like high triglycerides or autoimmune pancreatitis, medical management is essential:
- Medications: Statins, fibrates, or other lipid-lowering medications may be prescribed to control triglyceride levels. Immunosuppressive medications may be required for autoimmune pancreatitis.
- Pancreatic enzyme replacement therapy: For individuals with chronic pancreatitis and digestive issues, pancreatic enzyme supplements can help manage malabsorption and improve digestion.
3. Surgery and Interventions
For individuals with gallstones, pancreatic duct obstructions, or severe scarring, surgical interventions may be necessary:
- Cholecystectomy (removal of the gallbladder) may be recommended for individuals with gallstone-induced pancreatitis.
- Surgical procedures to clear pancreatic duct obstructions or remove cysts or tumors can prevent future episodes.
4. Regular Monitoring
For those with genetic predispositions, autoimmune conditions, or chronic pancreatitis, regular monitoring by a healthcare provider is essential to detect and address any signs of recurrent inflammation early. Regular imaging tests and blood work can help identify complications and prevent further damage.
The recurrence of pancreatitis is a multifaceted issue that is influenced by a variety of factors, including lifestyle choices, underlying medical conditions, and genetic predispositions. Managing recurrent pancreatitis requires addressing the root causes, whether it be alcohol consumption, gallstones, elevated triglycerides, or autoimmune diseases. By making necessary lifestyle changes, adhering to prescribed medications, and seeking timely medical intervention, individuals can reduce the risk of recurrent pancreatitis and improve their overall quality of life.
With proper management and preventive measures, individuals affected by pancreatitis can lead healthier, more fulfilling lives while minimizing the risk of future episodes.