1. Primary Sclerosing Cholangitis (PSC)
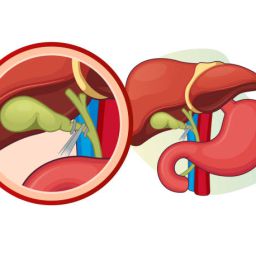
Primary sclerosing cholangitis (PSC) is a chronic, progressive disease that causes inflammation and fibrosis of the bile ducts. Over time, PSC leads to bile duct strictures, which can result in a complete blockage of bile flow. The exact cause of PSC is unknown, but it is commonly associated with autoimmune diseases, particularly ulcerative colitis.
How PSC Leads to Bile Duct Stricture
PSC causes inflammation and scarring in the bile ducts, leading to narrowing (strictures). This progressive scarring obstructs bile flow, causing a backup of bile in the liver. The condition is typically diagnosed in adults, and it may progress slowly over many years.
Symptoms of PSC
- Jaundice: A yellowing of the skin and eyes due to bile buildup.
- Fatigue: A common symptom due to the liver’s reduced ability to process toxins.
- Pruritus (Itchy Skin): Often a result of bile salts accumulating under the skin.
- Dark Urine: Due to excess bilirubin being processed by the kidneys.
- Abdominal Pain: Particularly in the upper right quadrant, due to bile duct obstruction.
Complications
- Cirrhosis: Progressive liver damage due to bile duct obstruction.
- Liver Failure: As the disease progresses, the liver may eventually fail.
- Cholangiocarcinoma: PSC significantly increases the risk of bile duct cancer.
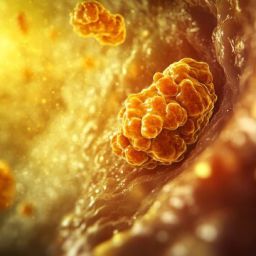
2. Bile Duct Cancer (Cholangiocarcinoma)

Cholangiocarcinoma, or bile duct cancer, is a rare but serious condition that can cause bile duct stricture. This cancer can develop in the bile ducts, blocking or narrowing them and impairing bile flow. Cholangiocarcinoma is most often diagnosed in individuals with long-standing liver disease or PSC.
How Cholangiocarcinoma Leads to Bile Duct Stricture
Cholangiocarcinoma causes the bile ducts to become blocked as the tumor grows, leading to a narrowing of the ducts. This obstruction can result in jaundice, infection, and other complications associated with bile flow disruption.
Symptoms of Cholangiocarcinoma
- Yellowing of the skin and eyes (jaundice)
- Abdominal pain: Often in the upper right abdomen.
- Unexplained weight loss
- Fever and chills: If an infection develops due to bile backup.
- Itchy skin (pruritus)
Treatment and Prognosis
Cholangiocarcinoma can be difficult to treat, particularly if diagnosed in its later stages. Treatment options include surgery, chemotherapy, and sometimes liver transplantation, but the prognosis tends to be poor due to the advanced nature of the disease at diagnosis.
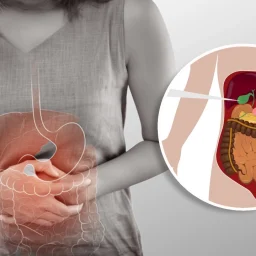
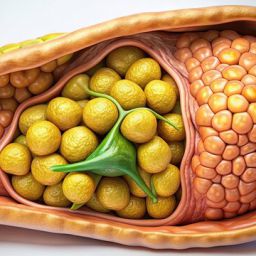
3. Gallstones and Biliary Obstruction
Gallstones are solid particles that form in the gallbladder and can migrate into the bile ducts, obstructing the normal flow of bile. When gallstones obstruct the bile duct, they can cause inflammation (cholangitis), which can result in scarring and the formation of strictures over time.
How Gallstones Lead to Bile Duct Stricture
If a gallstone becomes lodged in the bile duct, it can cause acute or chronic inflammation. Chronic inflammation can lead to fibrosis and scarring, which narrows the bile ducts and causes strictures.
Symptoms of Gallstone-Induced Bile Duct Obstruction
- Severe abdominal pain: Typically after eating fatty foods, which can indicate a blockage.
- Jaundice
- Fever and chills: Indicating possible cholangitis.
- Nausea and vomiting
Treatment
Treatment of gallstone-related bile duct strictures often involves removing the gallstone through endoscopic retrograde cholangiopancreatography (ERCP) or surgery. In some cases, stent placement or other interventions may be required to address the stricture.
4. Autoimmune Diseases

In addition to PSC, other autoimmune diseases can also cause bile duct stricture by triggering inflammation in the bile ducts. Autoimmune hepatitis and systemic lupus erythematosus (SLE) are examples of autoimmune conditions that can affect the liver and biliary system.
How Autoimmune Diseases Lead to Bile Duct Stricture
Autoimmune diseases occur when the body’s immune system mistakenly attacks its own tissues. In autoimmune hepatitis, the liver is damaged by the immune system, leading to inflammation of the bile ducts. In conditions like SLE, systemic inflammation can affect multiple organs, including the liver and bile ducts, leading to bile duct stricture.
Symptoms of Autoimmune-Related Bile Duct Strictures
- Fatigue: Often chronic and associated with autoimmune diseases.
- Jaundice
- Abdominal pain: Due to liver inflammation.
- Elevated liver enzymes: Indicative of liver damage.
Treatment
Autoimmune diseases that affect the bile ducts are often treated with immunosuppressive medications, such as corticosteroids, to reduce inflammation and prevent further damage. In some cases, additional treatments may be required, including liver transplantation in severe cases.
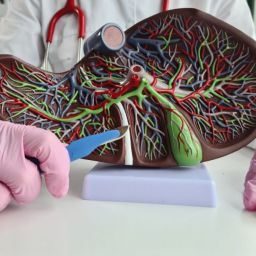
5. Primary Biliary Cholangitis (PBC)
Primary biliary cholangitis (PBC) is a chronic autoimmune disease that causes progressive damage to the small bile ducts in the liver. The disease leads to the destruction of these ducts, causing bile to accumulate in the liver and resulting in liver damage and eventual scarring.
How PBC Leads to Bile Duct Stricture
In PBC, the immune system targets and destroys the small bile ducts within the liver, leading to cholestasis (reduced bile flow) and the development of bile duct strictures. Over time, the liver becomes scarred, and cirrhosis may develop.
Symptoms of PBC
- Fatigue: One of the most common and debilitating symptoms.
- Jaundice: Yellowing of the skin and eyes.
- Itchy skin: Due to the buildup of bile acids in the skin.
- Dark urine and light-colored stools.
Treatment
PBC is treated with medications such as ursodeoxycholic acid (UDCA), which helps improve bile flow and prevent further liver damage. In severe cases, liver transplantation may be necessary.
6. Infection-Induced Cholangitis
Infections, particularly ascending cholangitis, can lead to bile duct stricture. This infection occurs when bacteria enter the bile ducts, often due to an obstruction such as a gallstone or tumor, and cause inflammation that can eventually result in fibrosis and narrowing of the ducts.
How Infection-Induced Cholangitis Leads to Bile Duct Stricture
The infection causes inflammation of the bile ducts, which may lead to scarring and narrowing over time. Chronic cholangitis can lead to persistent damage, and in severe cases, it may result in the formation of bile duct strictures.
Symptoms of Infection-Induced Cholangitis
- Fever and chills: Indicating the presence of infection.
- Jaundice
- Right upper abdominal pain
- Nausea and vomiting
Treatment
Infection-induced cholangitis is treated with antibiotics to address the bacterial infection. In some cases, procedures like ERCP may be necessary to remove the obstruction or place a stent to relieve the stricture.
7. Trauma or Surgical Injury
Trauma or surgical procedures that involve the bile ducts can lead to scarring and strictures. Bile duct injury during surgery, especially procedures like cholecystectomy (gallbladder removal), can cause bile duct narrowing. The risk of strictures is higher when the bile duct is accidentally cut or injured during surgery.
How Surgical Injury Leads to Bile Duct Stricture
When the bile duct is injured during surgery or trauma, scar tissue may form as part of the healing process. Over time, this scar tissue can cause the bile duct to narrow, leading to a stricture.
Symptoms of Surgical Injury-Induced Bile Duct Stricture
- Abdominal pain after surgery
- Jaundice: Due to bile backup.
- Fatigue and digestive issues due to impaired bile flow.
Treatment
Treatment may involve procedures to repair the injured bile duct, such as bile duct reconstruction or the placement of a stent to bypass the stricture.
Bile duct stricture is a serious condition that can arise from a variety of diseases. Whether caused by autoimmune disorders, infections, cancer, or trauma, bile duct strictures can lead to severe complications if left untreated. The condition requires prompt diagnosis and appropriate management, which may include medications, endoscopic procedures, or surgery. By understanding the diseases that cause bile duct strictures, individuals and healthcare providers can better manage this challenging condition and reduce the risk of long-term complications, including liver damage and failure.