The Role of the Pancreas in Blood Sugar Regulation
Before understanding how high sugar intake affects the pancreas, it is essential to understand the organ’s role in regulating blood sugar. The pancreas is located behind the stomach and is responsible for secreting important digestive enzymes and hormones. The two main hormones secreted by the pancreas that are involved in blood sugar regulation are insulin and glucagon.
- Insulin: After eating, the body absorbs glucose (sugar) from food, which enters the bloodstream. In response to rising blood sugar levels, the pancreas releases insulin. Insulin helps cells absorb glucose, allowing the body to use it as energy or store it for later use. It also helps maintain normal blood sugar levels by preventing excessive glucose buildup in the blood.
- Glucagon: When blood sugar levels drop too low, the pancreas releases glucagon, which signals the liver to release stored glucose back into the bloodstream. This hormone ensures that the body maintains a stable level of blood sugar, especially between meals or during physical activity.
Together, insulin and glucagon work to keep blood sugar levels within a narrow range. This delicate balance is crucial for overall health, as fluctuations in blood sugar can lead to a variety of metabolic disorders.
How High Sugar Consumption Affects the Pancreas
While the pancreas is equipped to handle fluctuations in blood sugar, consistent overconsumption of sugar can overwhelm the organ’s ability to function efficiently. Over time, excessive sugar intake can have several negative impacts on the pancreas.
1. Increased Insulin Production
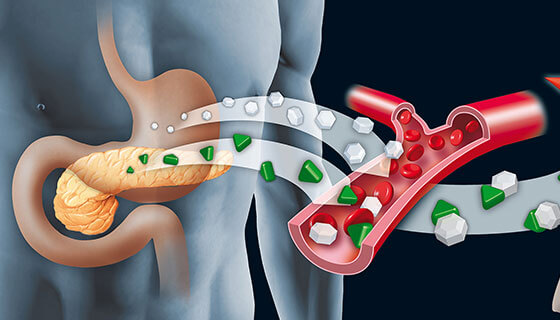
One of the most immediate effects of consuming large amounts of sugar is an increase in insulin production. When we eat sugary foods or drinks, the body experiences a rapid rise in blood glucose levels. In response, the pancreas releases insulin to help cells absorb glucose and return blood sugar levels to normal. However, if sugar consumption is consistently high, the pancreas has to release large amounts of insulin regularly to cope with the influx of glucose.
Over time, this increased demand for insulin production can lead to insulin resistance. Insulin resistance occurs when the body’s cells become less responsive to insulin, requiring even more insulin to achieve the same effect. The pancreas works overtime to produce more insulin, and eventually, it can become fatigued, leading to impaired insulin secretion.
2. Insulin Resistance and the Development of Type 2 Diabetes
Chronic high sugar intake is one of the primary contributors to insulin resistance. As the pancreas continues to pump out insulin in response to excess sugar, the body’s cells begin to lose their sensitivity to the hormone. This leads to a vicious cycle: the pancreas must produce more insulin to overcome resistance, which in turn leads to higher blood sugar levels and further strain on the pancreas.
If left unchecked, insulin resistance can lead to the development of type 2 diabetes. In this condition, the pancreas becomes unable to produce enough insulin to regulate blood sugar, leading to consistently high blood sugar levels. High blood sugar, also known as hyperglycemia, can have serious long-term health consequences, including heart disease, nerve damage, and kidney disease.
3. Fatty Liver and Pancreatic Dysfunction
Excessive sugar consumption, particularly fructose (a type of sugar found in many processed foods and sugary drinks), can lead to the accumulation of fat in the liver. This condition, known as non-alcoholic fatty liver disease (NAFLD), is strongly linked to insulin resistance and metabolic dysfunction. As the liver becomes overwhelmed with fat, it interferes with the pancreas’ ability to function properly.
When the liver is fatty and dysfunctional, it can impair insulin sensitivity, further exacerbating the strain on the pancreas. The pancreas struggles to produce enough insulin to compensate for the liver’s inability to process glucose, and as a result, blood sugar levels remain elevated.
4. Inflammation and Oxidative Stress
Consuming large amounts of sugar leads to inflammation and oxidative stress, both of which can damage the pancreas over time. High sugar levels trigger the release of inflammatory molecules in the body, contributing to chronic low-grade inflammation. This inflammation can directly affect pancreatic cells, making it more difficult for the organ to regulate blood sugar and produce insulin.
Furthermore, excessive sugar intake leads to the production of reactive oxygen species (ROS), which are highly reactive molecules that cause oxidative stress. Oxidative stress damages cells and tissues, including those in the pancreas, leading to impaired function and, potentially, pancreatic cell death.
The Long-Term Effects of High Sugar Consumption on the Pancreas
The long-term effects of chronic high sugar consumption on the pancreas can be severe and can lead to various metabolic disorders. Here are some of the most notable long-term consequences:
1. Increased Risk of Type 2 Diabetes

As mentioned earlier, high sugar consumption is one of the primary causes of insulin resistance, which can ultimately lead to the development of type 2 diabetes. This condition is characterized by the inability of the pancreas to produce sufficient insulin to regulate blood sugar levels effectively. The pancreas may initially compensate for the increased demand for insulin, but over time, it becomes exhausted and less able to produce the necessary amount of insulin.
Type 2 diabetes is a chronic condition that requires lifelong management, and it can lead to severe complications such as heart disease, kidney failure, nerve damage, and blindness if left untreated.
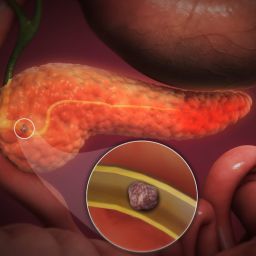
2. Pancreatic Fatty Infiltration and Dysfunction
Excess sugar, particularly fructose, can lead to the accumulation of fat in the pancreas, a condition known as pancreatic steatosis or fatty pancreas. Fatty infiltration of the pancreas can impair its ability to secrete insulin, making it more difficult for the body to regulate blood sugar levels. This can further contribute to the development of insulin resistance and type 2 diabetes.
Fatty infiltration of the pancreas is also associated with an increased risk of pancreatitis, a condition characterized by inflammation of the pancreas. Chronic pancreatitis can damage the pancreas permanently and may lead to pancreatic insufficiency, where the pancreas is no longer able to produce sufficient digestive enzymes or insulin.
3. Increased Risk of Metabolic Syndrome
Metabolic syndrome is a cluster of conditions that increase the risk of heart disease, stroke, and diabetes. High sugar consumption is one of the key contributors to metabolic syndrome, as it leads to obesity, insulin resistance, and high blood pressure.
The pancreas is at the center of metabolic syndrome, as insulin resistance often leads to elevated insulin levels, which in turn promote fat storage, particularly around the abdomen. This abdominal fat further exacerbates insulin resistance and creates a cycle of worsening metabolic health.
4. Damage to the Beta Cells in the Pancreas
The beta cells in the pancreas are responsible for producing insulin. Chronic high sugar consumption can lead to damage to these beta cells, impairing their ability to secrete insulin. Over time, the pancreas may become less efficient at regulating blood sugar, which contributes to the development of insulin resistance and diabetes.
In extreme cases, damage to the beta cells can lead to pancreatic beta-cell dysfunction, which is a major factor in the development of type 2 diabetes.
How to Protect the Pancreas and Mitigate the Impact of Sugar
While high sugar consumption can have damaging effects on the pancreas, there are several ways to protect the organ and promote better pancreatic health. Here are some strategies to mitigate the impact of sugar on the pancreas:

1. Reduce Sugar Intake
The most effective way to protect the pancreas is to reduce the intake of sugar, particularly added sugars found in processed foods and sugary beverages. By limiting sugar consumption, you can reduce the strain on the pancreas and improve insulin sensitivity.
2. Focus on Whole Foods
Eating a diet rich in whole foods, such as fruits, vegetables, whole grains, and lean proteins, can help support pancreatic health. These foods are nutrient-dense and provide the vitamins, minerals, and fiber necessary for optimal digestion and blood sugar regulation.
3. Incorporate Healthy Fats and Proteins
Healthy fats, such as those found in avocados, nuts, and olive oil, can help regulate blood sugar levels and improve insulin sensitivity. Additionally, consuming adequate amounts of protein can help stabilize blood sugar and support the pancreas in its insulin production.
4. Engage in Regular Physical Activity
Exercise plays a crucial role in maintaining healthy blood sugar levels and improving insulin sensitivity. Regular physical activity helps the body use insulin more efficiently and reduces the risk of developing insulin resistance and type 2 diabetes.
5. Manage Stress
Chronic stress can worsen insulin resistance and contribute to the development of metabolic disorders. Practicing stress-reducing techniques such as meditation, deep breathing exercises, or yoga can help support pancreatic function.
The pancreas is essential for maintaining healthy blood sugar levels, and excessive sugar consumption can severely impact its function. Over time, chronic high sugar intake can lead to insulin resistance, fatty infiltration of the pancreas, and an increased risk of type 2 diabetes and metabolic syndrome. By reducing sugar intake, focusing on a healthy diet, and engaging in regular physical activity, individuals can protect their pancreas and improve overall metabolic health. By taking proactive steps now, you can help prevent long-term damage to the pancreas and reduce your risk of developing serious health conditions in the future.