The Relationship Between Gallstones and Pancreatitis
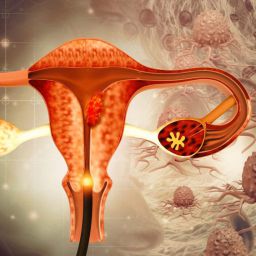
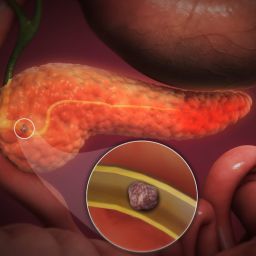
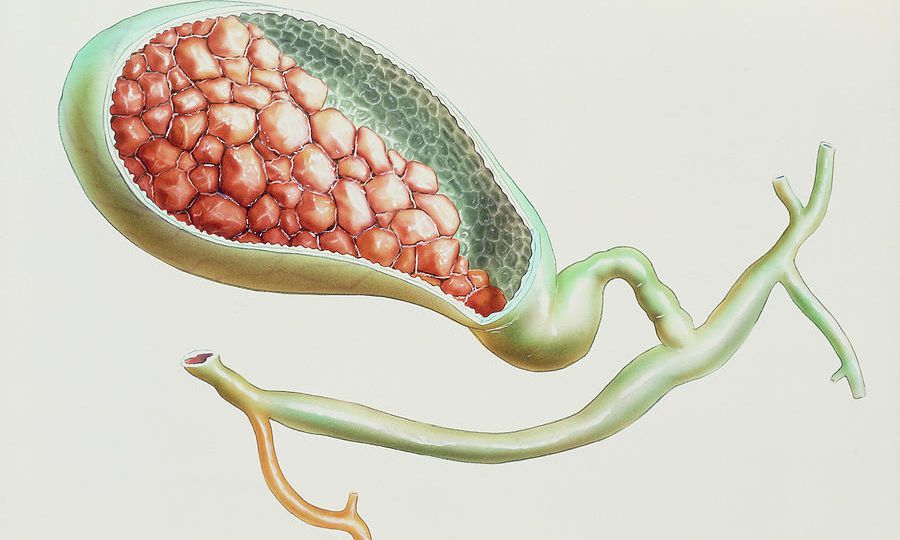
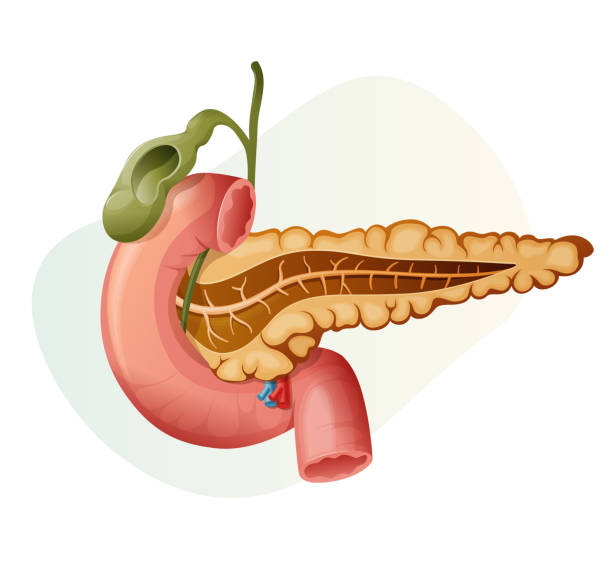
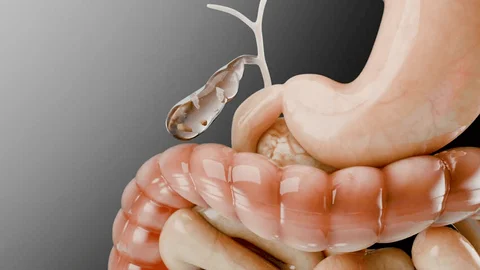
The pancreas and the gallbladder are closely linked anatomically and functionally. The gallbladder stores bile, a substance that helps digest fats, and releases it into the small intestine through the common bile duct. The pancreas also has a duct (the pancreatic duct) that releases digestive enzymes into the small intestine. These two ducts meet at the ampulla of Vater, a crucial junction where both bile and pancreatic enzymes are released simultaneously into the small intestine. When gallstones enter the bile duct and obstruct this passage, it can create a backup of bile and digestive enzymes. This blockage can lead to the inflammation of the pancreas, which is known as gallstone-induced pancreatitis.
Mechanisms of Gallstone-Induced Pancreatitis
Gallstones can lead to pancreatitis in two primary ways:
- Obstruction of the Bile Duct: Gallstones can block the bile duct, preventing bile from flowing from the gallbladder into the small intestine. This obstruction can increase pressure in the bile ducts and lead to the release of bile into the pancreas, which can trigger inflammation and pancreatitis.
- Obstruction of the Pancreatic Duct: A gallstone can also enter the pancreatic duct, blocking the flow of digestive enzymes. This obstruction can cause the enzymes to back up into the pancreas, leading to premature activation and resulting in self-digestion of the pancreas, which causes inflammation.
In both cases, the end result is acute pancreatitis, a condition marked by sudden and severe inflammation of the pancreas.
Risk Factors for Gallstone-Induced Pancreatitis
While not everyone with gallstones will develop pancreatitis, several risk factors increase the likelihood of a person experiencing gallstone-induced pancreatitis:
- Size of the Gallstones: Larger gallstones are more likely to obstruct the bile duct and pancreatic duct, increasing the risk of pancreatitis.
- Multiple Gallstones: The presence of several smaller gallstones may raise the chances of one getting lodged in the ducts, causing obstruction.
- Age: The incidence of gallstones increases with age, and older individuals are at higher risk for developing complications like pancreatitis.
- Gender: Women, especially those who are overweight or have a history of pregnancy, are more likely to develop gallstones compared to men.
- Obesity: Obesity is a significant risk factor for gallstone formation, and it can increase the likelihood of pancreatitis as well.
- Rapid Weight Loss: Rapid weight loss, often through surgery or extreme dieting, can increase the risk of gallstones. These stones may cause complications if they migrate into the ducts.
- Diabetes: People with diabetes are at an elevated risk for gallstones and, consequently, pancreatitis.
Symptoms of Gallstone-Induced Pancreatitis
The symptoms of gallstone-induced pancreatitis often resemble those of other forms of pancreatitis but may include additional signs related to the gallbladder. Common symptoms of gallstone-related pancreatitis include:
- Severe Upper Abdominal Pain: This pain typically starts suddenly and can be intense, often radiating to the back. It is usually worse after eating fatty foods.
- Jaundice: If a gallstone obstructs the bile duct, it can cause a buildup of bilirubin in the body, leading to yellowing of the skin and eyes (jaundice).
- Nausea and Vomiting: Persistent nausea and vomiting are common in cases of pancreatitis, especially in the acute phase.
- Fever and Chills: When infection is present, a person may develop a fever and experience chills.
- Bloating and Indigestion: As the digestive system becomes compromised due to the obstruction, bloating and indigestion may occur.
If you experience any of these symptoms, it is crucial to seek medical attention immediately, as untreated pancreatitis can escalate into severe complications, including organ failure.
Diagnosis of Gallstone-Induced Pancreatitis
To diagnose gallstone-induced pancreatitis, healthcare providers rely on a combination of medical history, physical examination, blood tests, and imaging studies.
- Blood Tests: Elevated levels of pancreatic enzymes, such as amylase and lipase, are common in acute pancreatitis. Additionally, liver enzyme levels may be elevated, indicating a possible obstruction in the bile duct caused by gallstones.
- Imaging Tests:
- Ultrasound: This non-invasive imaging technique is often the first choice to detect gallstones in the gallbladder and bile ducts.
- CT Scan: A CT scan provides detailed images of the pancreas and surrounding organs, helping doctors assess the extent of the inflammation and detect complications.
- MRI: Magnetic resonance imaging (MRI) can be used to get clear images of the bile and pancreatic ducts.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): ERCP is a specialized procedure that involves using an endoscope to examine the bile and pancreatic ducts. It can also be used to remove gallstones causing the blockage and relieve the obstruction.
- Endoscopic Ultrasound (EUS): This test is particularly useful for detecting small gallstones or other abnormalities in the bile and pancreatic ducts.
Treatment Options for Gallstone-Induced Pancreatitis
The treatment for gallstone-induced pancreatitis typically depends on the severity of the condition, the underlying cause, and the presence of complications. The primary focus is to manage the inflammation, relieve the blockage, and address any infections.
- Hospitalization and Supportive Care: In most cases, people with pancreatitis are hospitalized for observation. Supportive care includes:
- Intravenous fluids to keep the body hydrated and support organ function.
- Pain management to alleviate severe abdominal pain.
- Nutritional support via an IV or feeding tube, especially if the person cannot eat for an extended period.
- Endoscopic Removal of Gallstones: If a gallstone is causing a blockage in the bile or pancreatic duct, an ERCP procedure can be performed to remove the stone. This is often the first line of treatment in cases of obstructive gallstone-induced pancreatitis.
- Cholecystectomy (Gallbladder Removal): Once the acute episode of pancreatitis is treated, patients may undergo cholecystectomy, a surgery to remove the gallbladder. This procedure is generally recommended to prevent future episodes of gallstone-related complications.
- Surgical Intervention: In rare cases where ERCP is unsuccessful or if there are complications such as abscesses or bile duct damage, surgery may be required to remove the gallstones or treat the affected organs.
- Antibiotics: If an infection is present, antibiotics may be prescribed to treat bacterial infections in the pancreas or bile ducts.
- Managing Complications: Severe pancreatitis can lead to complications like abscesses, sepsis, or organ failure, which may require intensive care and more aggressive treatment.
Preventive Measures for Gallstone-Induced Pancreatitis
While not all cases of pancreatitis can be prevented, several steps can be taken to reduce the risk of gallstones and pancreatitis:
- Maintain a Healthy Diet: Eating a balanced, low-fat diet rich in fiber can reduce the risk of developing gallstones. Foods like fruits, vegetables, whole grains, and healthy fats should be included in your diet.
- Maintain a Healthy Weight: Obesity is a major risk factor for gallstones, so maintaining a healthy weight through regular physical activity and a balanced diet is crucial.
- Avoid Rapid Weight Loss: Losing weight too quickly can increase the risk of gallstone formation, so it is advisable to adopt a gradual weight loss approach.
- Exercise Regularly: Regular physical activity helps maintain a healthy weight and reduces the risk of gallstones. Aim for at least 30 minutes of moderate exercise most days of the week.
- Limit Alcohol Consumption: Excessive alcohol consumption can lead to liver damage and increase the risk of gallstones and pancreatitis. Limiting or avoiding alcohol can help reduce this risk.
- Manage Underlying Health Conditions: If you have diabetes, high cholesterol, or other conditions that predispose you to gallstones, working with your healthcare provider to manage these conditions can reduce the risk of gallstone-related pancreatitis.
Gallstones are a significant risk factor for the development of pancreatitis, particularly when they obstruct the bile or pancreatic ducts. While not everyone with gallstones will develop pancreatitis, the condition can be severe and potentially life-threatening when it occurs. If you have gallstones or suspect you may have pancreatitis, seek medical attention immediately to prevent complications. Early intervention can help alleviate symptoms and reduce the risk of further damage to the pancreas. By understanding the relationship between gallstones and pancreatitis, individuals can take preventive measures and make informed decisions about their health.