1. Appendicitis During Pregnancy: A Unique Challenge
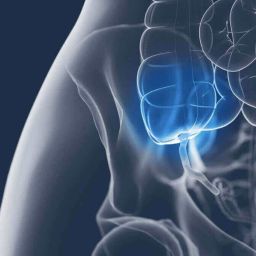
Pregnant women are more susceptible to appendicitis due to changes in their body during pregnancy, including hormonal changes and the physical shifts that occur as the pregnancy progresses. Appendicitis during pregnancy, while not overly common, represents a unique medical challenge. The diagnosis and management of appendicitis in pregnant women require careful consideration because of the potential impact on both the mother’s health and the developing fetus.
a. Symptoms of Appendicitis in Pregnant Women
The symptoms of appendicitis in pregnant women can be more difficult to identify compared to non-pregnant individuals. The classic symptoms of appendicitis include abdominal pain, nausea, vomiting, and fever. However, these symptoms can overlap with other pregnancy-related issues such as morning sickness, indigestion, and round ligament pain, leading to delayed diagnosis.
- Abdominal Pain: In non-pregnant individuals, pain from appendicitis typically begins around the belly button and later moves to the lower right side of the abdomen. In pregnant women, however, as the pregnancy progresses, the appendix moves up and to the right side of the abdomen, making it harder to pinpoint the location of pain.
- Nausea and Vomiting: Nausea and vomiting are common during pregnancy, especially in the first trimester, which can make it difficult to differentiate between appendicitis and morning sickness.
- Fever: Fever is often present with appendicitis, but it can be harder to detect in pregnancy since low-grade fever is sometimes a normal occurrence due to hormonal changes.
Because appendicitis can be difficult to diagnose in pregnant women, it is crucial for healthcare providers to consider the possibility of appendicitis early on, especially if a woman has persistent abdominal pain that does not resolve on its own.
b. Diagnostic Challenges
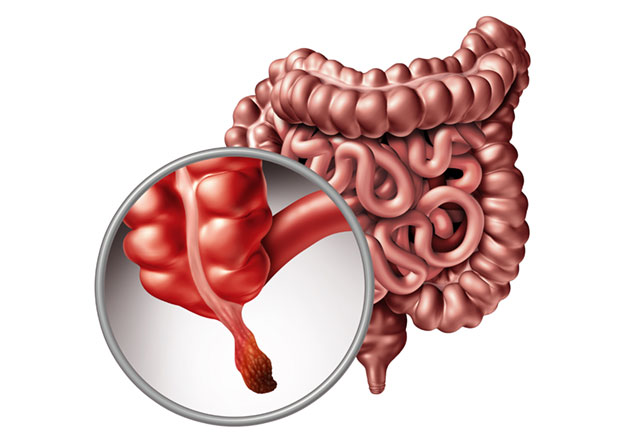
In the case of suspected appendicitis during pregnancy, healthcare providers must consider several factors when deciding on the diagnostic approach. Imaging tests such as ultrasound and MRI are typically used, as they do not expose the fetus to harmful radiation. However, there are some challenges with imaging:
- Ultrasound: Ultrasound is commonly used in pregnancy to diagnose appendicitis. It is generally safe for the fetus, but it can sometimes be challenging to obtain clear images, particularly in the later stages of pregnancy due to the presence of the uterus.
- MRI: Magnetic Resonance Imaging (MRI) is another safe alternative during pregnancy. MRI provides detailed images without radiation and can help diagnose appendicitis accurately.
- CT Scan: A CT scan is not typically recommended during pregnancy because it involves exposure to radiation, which can be harmful to the fetus, especially in the first trimester. However, in some cases, where the diagnosis is uncertain and other imaging methods have failed, a CT scan may be used, but only after weighing the risks and benefits.
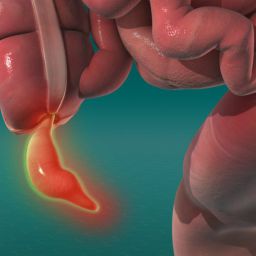
Timely diagnosis is crucial because delayed treatment can lead to the rupture of the appendix, which poses significant risks for both the mother and the fetus.
2. Risks of Appendectomy During Pregnancy
If appendicitis is confirmed, appendectomy is the standard treatment. However, the procedure carries certain risks, particularly when performed during pregnancy. The primary risks associated with appendectomy during pregnancy can be divided into maternal risks and fetal risks.
a. Risks for the Mother
The risks to the mother during appendectomy are similar to those for non-pregnant individuals, including:
- Infection: Infection is a risk for any surgical procedure, including appendectomy. If the appendix has ruptured before the surgery, the risk of infection increases significantly.
- Anesthesia Complications: Anesthesia carries risks, especially during pregnancy. The type of anesthesia used during the surgery must be carefully considered to avoid complications for the mother and baby. General anesthesia is commonly used, but it can affect the pregnancy depending on the trimester.
- Bleeding: Although rare, excessive bleeding can occur during surgery. The pregnancy can also make it more difficult for the surgeon to control bleeding due to the altered physiology of pregnant women, such as changes in blood flow and blood pressure.
Despite these risks, appendectomy is typically considered to be safer than leaving the condition untreated, as untreated appendicitis can result in sepsis, peritonitis, or even maternal death.
b. Risks for the Fetus
The risks for the fetus during appendectomy largely depend on the stage of pregnancy, the timing of surgery, and how quickly the mother receives treatment. Some of the key fetal risks include:
- Premature Labor: Surgery during pregnancy can increase the risk of premature labor, especially if the appendix has ruptured. Premature delivery can lead to complications for the baby, including respiratory distress syndrome, low birth weight, and long-term developmental issues.
- Injury to the Fetus: In rare cases, surgical procedures on pregnant women can lead to direct injury to the fetus, especially if there are complications during surgery or if the pregnancy is advanced.
- Fetal Distress: General anesthesia and the stress of surgery can lead to fetal distress, particularly in the second and third trimesters. Monitoring of the fetal heart rate is essential during and after surgery.
To minimize these risks, it is important for the surgical team to work closely with obstetricians and pediatric specialists to provide optimal care during the procedure.
3. Timing of Appendectomy During Pregnancy
The timing of appendectomy during pregnancy plays a critical role in minimizing risks to both the mother and the fetus. The approach to appendicitis varies depending on the stage of pregnancy and the severity of the condition.
a. First Trimester

In the first trimester, the risks to the fetus are highest due to the early development of the baby’s organs. However, appendicitis during the first trimester should still be treated immediately to avoid complications like rupture and peritonitis, which can be fatal to the mother. Laparoscopic surgery is usually preferred in the first trimester because it is minimally invasive, reduces the risk of infection, and has a shorter recovery time compared to open surgery.
b. Second Trimester
The second trimester is considered the safest period for performing surgery during pregnancy. The baby’s organs are fully developed, and the risk of miscarriage or preterm labor is lower compared to the first and third trimesters. At this stage, laparoscopic appendectomy is generally the preferred method as it minimizes the risk of complications for both the mother and the fetus.
c. Third Trimester
The third trimester presents more challenges for appendectomy. The growing uterus can make it more difficult for the surgeon to access the appendix, and the risk of preterm labor increases. However, if appendicitis occurs during the third trimester, surgery is still necessary to prevent complications like rupture, as the risks of leaving the condition untreated far outweigh the risks of surgery. In some cases, open appendectomy may be required due to the physical changes in the abdomen.
4. Management and Post-Surgical Care for Pregnant Women
After undergoing an appendectomy during pregnancy, the mother will require careful monitoring and post-operative care to ensure her safety and the well-being of the fetus.
a. Post-Surgical Care
Following appendectomy, the mother will typically be monitored in the hospital for a few days to ensure that there are no complications such as infection, bleeding, or preterm labor. Pain management is an important aspect of post-operative care. Medications used for pain relief must be carefully chosen to avoid any harm to the fetus.
b. Fetal Monitoring
Continuous fetal monitoring is essential, especially if the surgery is performed in the second or third trimester. The fetal heart rate will be closely monitored during and after surgery to detect any signs of distress.
c. Recovery and Follow-Up Care
After being discharged from the hospital, the mother should follow-up regularly with both the surgeon and the obstetrician to ensure proper healing. Physical rest, avoiding heavy lifting, and staying hydrated are important aspects of recovery. Additionally, the mother should be vigilant for any signs of infection or complications, such as fever, severe abdominal pain, or changes in fetal movement.
While appendectomy during pregnancy does carry certain risks, it is generally considered to be safe when performed by an experienced surgical team and with careful management. Timely diagnosis and treatment of appendicitis are critical to preventing complications, such as rupture and peritonitis, which pose a greater risk to both the mother and the baby. With the right approach, the risks associated with appendectomy can be minimized, and both the mother and baby can have a good outcome.
Ultimately, the decision to perform an appendectomy during pregnancy depends on a variety of factors, including the stage of pregnancy, the severity of appendicitis, and the overall health of the mother and fetus. By working closely with a multidisciplinary team of healthcare providers, pregnant women with appendicitis can receive the best possible care to ensure a safe and healthy recovery for both themselves and their unborn child.