1. Understanding Anal Fissures: A Brief Overview
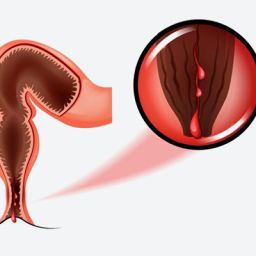
An anal fissure is a small tear or cut in the skin around the anus. It typically occurs when the anal sphincter, the muscle responsible for controlling bowel movements, is stretched beyond its normal capacity, often due to the passage of hard or large stools. Other causes can include chronic diarrhea, childbirth, or anal trauma. Anal fissures can be either acute (newly formed) or chronic (long-standing and persistent).
Symptoms of Anal Fissures
The primary symptom of an anal fissure is pain, particularly during and after a bowel movement. This pain can be sharp and intense, often lasting for several minutes or even hours after defecation. Other symptoms may include:

- Bright red blood on toilet paper or in the toilet bowl after a bowel movement
- Itching or irritation around the anus
- Swelling or a small lump near the fissure site
- A visible tear or crack in the skin around the anus, which can sometimes be seen upon examination
While anal fissures are usually not serious, they can cause significant discomfort and may lead to further complications if not treated effectively.
2. Why Anal Fissures Need to Be Treated Promptly
Most anal fissures will heal on their own within a few days to weeks with the right care, such as dietary changes, stool softeners, and proper hygiene. However, if left untreated or improperly managed, anal fissures can develop into chronic conditions, resulting in long-term health issues and complications that can significantly affect the quality of life.
3. Risks of Untreated Anal Fissures
When an anal fissure is left untreated, the condition can worsen over time and lead to several risks and complications. Some of these include:
3.1 Chronic Anal Fissures
One of the most significant risks of untreated anal fissures is the progression to a chronic condition. An acute anal fissure typically heals within a few weeks with appropriate treatment. However, if a fissure is not properly managed, it can become chronic, meaning it lasts for more than six weeks or recurs frequently.
Chronic anal fissures can be more difficult to treat and may require more invasive treatment methods. They can also lead to ongoing pain and discomfort, affecting daily activities and overall well-being.
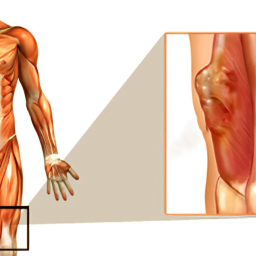
3.2 Anal Fissure with an Internal Anal Sphincter Spasm
The anal sphincter is the muscle responsible for controlling bowel movements, and it plays a key role in the healing of anal fissures. When an anal fissure is not treated promptly, the muscle around the fissure may go into spasm in response to the pain, which can make it even more difficult for the fissure to heal. This creates a vicious cycle where the spasm leads to more pain, preventing healing, and further exacerbating the condition.
The presence of spasms in the internal anal sphincter can delay healing and increase the risk of chronic fissures. In severe cases, this can lead to complications that may require surgical intervention to resolve.
3.3 Infection Risk
An untreated anal fissure increases the risk of infection, especially if the tear becomes deeper or more extensive. The anus is home to many bacteria, and when the skin is broken, bacteria can enter the wound and cause an infection.
Infections in the area around an anal fissure can lead to abscess formation, which is a pocket of pus that can cause further pain, swelling, and discomfort. Abscesses may require drainage and sometimes antibiotics to treat the infection. In rare cases, untreated abscesses can lead to more severe infections or sepsis, a life-threatening condition that requires immediate medical attention.
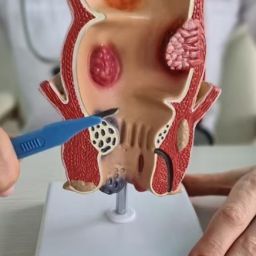
3.4 Development of Anal Fistulas
A fistula is an abnormal connection between two body parts, such as the anus and the skin. If an anal fissure is left untreated for a long time, it may lead to the formation of an anal fistula. This occurs when the fissure extends deep enough to form a tunnel under the skin, linking the anal canal to the skin near the anus.
Anal fistulas are typically accompanied by painful abscesses, leakage of stool or pus, and recurrent infections. They can be challenging to treat and often require surgery to repair the fistula and prevent further complications.
3.5 Rectal Prolapse
In some cases, chronic anal fissures can lead to rectal prolapse, a condition where part of the rectum protrudes through the anus. This is more likely to occur in individuals who frequently strain during bowel movements or have chronic constipation. Rectal prolapse is not only painful but can also result in additional complications such as fecal incontinence (inability to control bowel movements).
4. How to Prevent Complications from Anal Fissures
To avoid the complications associated with untreated anal fissures, it is important to adopt strategies for preventing the fissures from developing or worsening. Here are some key preventative measures:

4.1 Increase Fiber Intake
One of the most effective ways to prevent anal fissures is to eat a high-fiber diet. Fiber helps to soften the stool, making it easier to pass without straining. This reduces the risk of tearing the sensitive skin around the anus. High-fiber foods include fruits, vegetables, whole grains, and legumes.
4.2 Stay Hydrated
Drinking plenty of water is essential to keeping stool soft and preventing constipation. Dehydration can lead to hard stools, which can increase the risk of developing anal fissures. Aim for at least eight glasses of water per day, and adjust your intake based on your activity level and climate.
4.3 Avoid Straining During Bowel Movements
Straining during bowel movements puts significant pressure on the anal area, which can lead to the development of fissures. To avoid this, it is important to go to the bathroom when you feel the urge, rather than holding it in. If constipation is an issue, consider using stool softeners or laxatives, but do so under the guidance of a healthcare professional.
4.4 Practice Proper Hygiene
Maintaining proper hygiene around the anal area is important to prevent infections and further irritation. After each bowel movement, gently clean the area with water and mild soap, avoiding harsh wipes or scented products that can cause irritation. Consider using moist wipes instead of dry toilet paper for more comfort.
4.5 Consider Warm Sitz Baths
Soaking in a warm sitz bath can help soothe the pain associated with anal fissures. This helps relax the muscles around the anus and promotes healing. Sitz baths should be done several times a day, especially after bowel movements, to alleviate discomfort and reduce inflammation.
4.6 Medical Treatment
If the fissure does not improve with conservative measures, or if it becomes chronic, medical treatment may be necessary. Topical medications, such as nitroglycerin ointment or calcium channel blockers, can help relax the anal sphincter and promote healing. In more severe cases, Botox injections or surgical options like lateral internal sphincterotomy may be considered.
Anal fissures, while common, should not be ignored. If left untreated, they can lead to chronic conditions, infections, abscesses, and even fistulas or rectal prolapse. Early detection and prompt treatment are essential to prevent these complications. By practicing proper hygiene, maintaining a healthy diet, staying hydrated, and seeking medical attention when necessary, individuals can minimize the risks and avoid the potentially serious consequences of untreated anal fissures.
If you are experiencing persistent pain, bleeding, or discomfort in the anal area, consult a healthcare professional for an accurate diagnosis and appropriate treatment. Taking action early can help you avoid complications and get back to your normal life with minimal disruption.