What Are the Potential Complications Caused by Liver Echinococcosis?
Liver echinococcosis, also known as hydatid disease, is caused by the parasitic tapeworm Echinococcus granulosus. This infection affects both humans and animals, with humans becoming infected through contact with eggs released by infected canines, particularly dogs. While the disease is endemic in many parts of the world, particularly in areas where livestock farming is common, the impact of liver echinococcosis on human health can be severe, resulting in a range of complications.
Echinococcosis primarily involves the formation of cysts in the liver, though it can affect other organs such as the lungs and brain. These cysts, which develop from the larvae of the Echinococcus parasite, can lead to numerous health issues depending on their size, location, and the presence of secondary infections.
Understanding the potential complications of liver echinococcosis is crucial for timely intervention and treatment. Left untreated, these complications can lead to organ failure, sepsis, or even death.
Development and Progression of Liver Echinococcosis
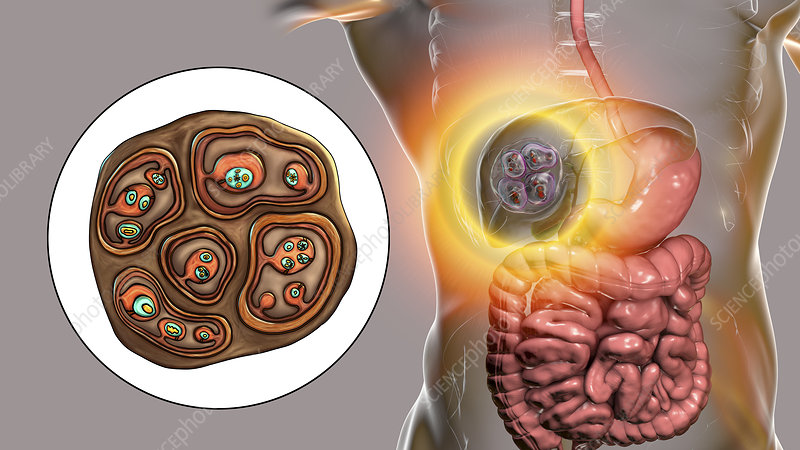
The pathogenesis of liver echinococcosis begins when a person ingests Echinococcus eggs, typically through contaminated food, water, or soil. Once ingested, the eggs hatch into larvae in the intestines and travel to the liver via the bloodstream. In the liver, the larvae grow into cysts, which can range in size from small, asymptomatic lesions to large, life-threatening masses.
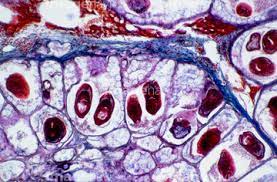
These cysts are filled with fluid and may contain numerous protoscolices, which are the infectious larvae that can later spread the disease if they rupture. Over time, the cysts can increase in size, putting pressure on surrounding tissues and organs, which leads to the onset of complications. The symptoms associated with these complications depend largely on the size, location, and stage of the cysts.
Potential Complications Caused by Liver Echinococcosis
1. Cyst Rupture
One of the most dangerous complications of liver echinococcosis is the rupture of the cyst. When a cyst ruptures, it can release its contents into the abdominal cavity, causing severe reactions such as anaphylaxis or peritonitis. The released cyst fluid may contain large numbers of protoscolices, leading to the development of secondary cysts in other organs. This is known as “dissemination” of the parasite and can significantly worsen the prognosis of the patient.
Rupture can occur spontaneously or due to trauma, such as a blow to the abdomen. This complication requires immediate medical attention, as the associated risks of sepsis and systemic infection can be life-threatening.
2. Biliary Obstruction
Large cysts located in the liver can cause mechanical obstruction of the bile ducts, leading to conditions such as jaundice or cholangitis. When bile flow is blocked, the liver’s ability to process bilirubin is impaired, causing a buildup of bilirubin in the bloodstream. This leads to the yellowing of the skin and eyes, a hallmark symptom of jaundice.
Cholangitis, an inflammation of the bile ducts, may also occur as a result of the obstruction. This condition is often characterized by fever, abdominal pain, and jaundice. In severe cases, it can progress to liver failure if not treated promptly.
3. Liver Dysfunction and Failure
In some cases, liver echinococcosis can cause progressive liver damage, leading to hepatic dysfunction or even liver failure. The presence of large cysts can disrupt normal liver tissue, leading to impaired hepatic function. This condition may manifest as weakness, fatigue, abdominal pain, and swelling due to fluid buildup (ascites).
If liver failure occurs, it may necessitate a liver transplant, particularly in cases where medical management and surgery are not sufficient to manage the damage.
4. Infection and Sepsis
Infections of the cysts themselves can occur, particularly if the cysts rupture or are punctured during diagnostic procedures. When the cysts become infected, they can lead to sepsis, a life-threatening systemic response to infection. Sepsis occurs when bacteria or toxins from the infected cysts enter the bloodstream, leading to widespread inflammation and organ dysfunction.
The signs of sepsis include fever, chills, rapid heartbeat, confusion, and low blood pressure. Sepsis requires immediate treatment with antibiotics and, in severe cases, organ support.
5. Hydatid Cyst Calcification
Over time, some echinococcal cysts may undergo calcification, where the cyst wall becomes hardened and filled with calcium deposits. Although calcified cysts are usually less symptomatic, they can still cause complications if they grow large enough to exert pressure on nearby organs.
Calcification may also make it difficult for healthcare providers to distinguish between a hydatid cyst and other types of liver tumors or cysts, complicating diagnosis and treatment decisions.
6. Secondary Cyst Formation in Other Organs
In cases where the cyst ruptures and releases protoscolices into the bloodstream, new cysts may form in other organs, including the lungs, kidneys, and brain. These secondary cysts can cause additional complications, depending on their location. For example, cysts in the lungs can lead to respiratory distress, while cysts in the brain may cause neurological symptoms such as headaches, seizures, or cognitive impairment.
Secondary cysts are a significant concern because they represent a spread of the infection to other parts of the body, making treatment more challenging.
7. Anaphylaxis
In rare cases, patients with liver echinococcosis may experience an allergic reaction to the contents of the cysts if they rupture. This reaction, known as anaphylaxis, can be severe and life-threatening. Symptoms of anaphylaxis include difficulty breathing, swelling of the face and throat, and a drop in blood pressure. Immediate medical intervention, including the administration of epinephrine, is necessary to treat this condition.
Diagnosis and Treatment of Liver Echinococcosis
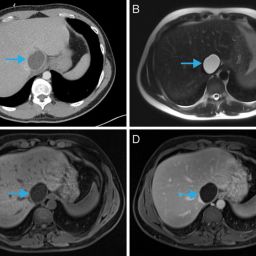
The diagnosis of liver echinococcosis typically involves imaging techniques such as ultrasound, CT scans, or MRI to visualize the cysts and assess their size, location, and characteristics. Blood tests may also be performed to detect antibodies against Echinococcus.
Treatment for liver echinococcosis depends on the size and location of the cysts, as well as the severity of the complications. Common treatment options include:
- Surgical Removal: Surgical intervention is often necessary to remove large cysts or when cyst rupture occurs. The procedure involves either removing the cyst or performing a procedure called “cystectomy,” where the cyst wall is carefully excised.
- Antiparasitic Medications: Drugs like albendazole or mebendazole are used to kill the parasite and prevent further cyst growth. These medications are often used in combination with surgery.
- Percutaneous Techniques: In some cases, percutaneous drainage or aspiration of the cysts may be used, particularly if surgery is not feasible.
- Liver Transplantation: In cases of severe liver damage or failure, liver transplantation may be considered.
Prevention of Liver Echinococcosis
Preventing liver echinococcosis relies on controlling the spread of Echinococcus and reducing human exposure to its eggs. Some preventive measures include:
- Proper Hygiene Practices: Regular handwashing and maintaining good hygiene are essential in preventing the ingestion of Echinococcus eggs.
- Control of Animal Populations: De-worming programs for dogs and other carnivores can significantly reduce the risk of transmission.
- Safe Food Handling: Ensuring that meat from livestock is properly cooked and avoiding consumption of undercooked meat is important for preventing the spread of Echinococcus.