How Do Liver Echinococcal Cysts Form?
The formation of liver echinococcal cysts follows a complex life cycle involving definitive and intermediate hosts. The primary host for Echinococcus species is typically a carnivorous animal such as a dog or wolf, while intermediate hosts are herbivores like sheep, cattle, and humans. Human infection occurs when a person accidentally ingests Echinococcus eggs, which are typically passed in the feces of infected carnivores.
Life Cycle of Echinococcosis:
- Eggs in the Environment: Adult tapeworms of Echinococcus species reside in the intestines of carnivores. These tapeworms release eggs through feces, which contaminate the environment. Humans can ingest these eggs by consuming contaminated food, water, or coming into contact with infected animals.
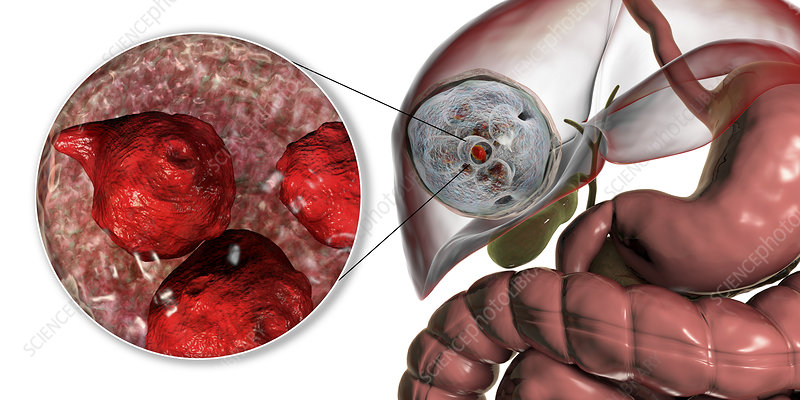
- Larvae Formation and Migration: Once ingested, the eggs hatch in the human digestive system, releasing larvae (oncospheres). These larvae penetrate the intestinal wall and enter the bloodstream, traveling to various organs. The liver is the most common site for these larvae to settle, where they begin to form cysts.
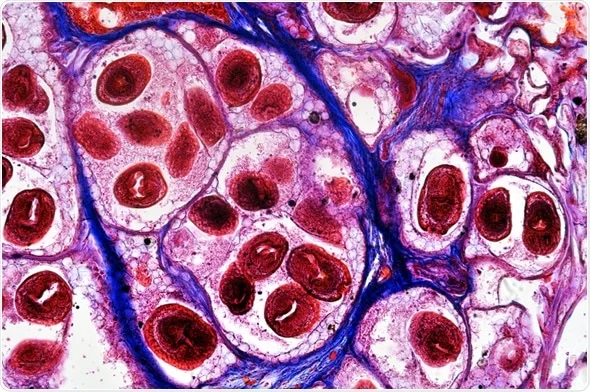
- Cyst Growth: The larvae grow into large, fluid-filled cysts over time. These cysts are usually slow-growing and may remain asymptomatic for years. The cyst walls can contain numerous protoscolices (larvae), which can spread and cause further infections if ruptured.
- Cyst Complications: In some cases, the cysts can grow to significant sizes, pressing against surrounding organs and causing various symptoms such as abdominal pain, jaundice, and nausea. If a cyst ruptures, it can lead to the spread of larvae to other areas of the body, causing life-threatening complications such as anaphylactic shock or peritonitis.
Risk Factors for Developing Liver Echinococcal Cysts
Several factors contribute to the development of liver echinococcal cysts. These factors are closely related to lifestyle, environment, and hygiene practices. Understanding these risk factors can help in the prevention and early detection of the disease.
- Geographical Location: Echinococcosis is more common in rural areas where people have close contact with livestock and domestic animals such as dogs. Regions such as parts of the Mediterranean, Central Asia, South America, and the Middle East are particularly affected due to agricultural practices and the presence of stray dogs. In these areas, people are more likely to be exposed to contaminated food, water, or direct contact with animals carrying the parasite.
- Exposure to Infected Animals: People who live or work with livestock or stray dogs are at an increased risk of infection. Infected dogs can spread the Echinococcus eggs to their environment, which may contaminate pastures, food, or water sources.
- Poor Hygiene Practices: Lack of proper hygiene, particularly in rural or undeveloped areas, increases the risk of Echinococcus transmission. This includes failure to wash hands after handling animals, eating unwashed fruits or vegetables, or drinking untreated water from contaminated sources.
- Environmental Factors: Environmental conditions, such as open grazing of livestock and inadequate waste disposal systems, also contribute to the spread of Echinococcus. These conditions create opportunities for contamination of the soil, water, and food that humans and animals may ingest.
- Immune System Status: Although rare, individuals with weakened immune systems, such as those with HIV/AIDS or those on immunosuppressive therapy, may be at greater risk for developing more severe forms of echinococcosis due to their bodies’ reduced ability to fight off infections.
Symptoms of Liver Echinococcal Cysts
Liver echinococcal cysts can remain asymptomatic for a long period, with patients often unaware that they are infected. The cysts may be small initially and grow slowly, making early diagnosis challenging. As the cysts grow in size and press against the liver and surrounding organs, they may cause symptoms such as:
- Abdominal Pain: Pain, particularly in the upper right quadrant of the abdomen, is the most common symptom. This pain occurs as the growing cysts exert pressure on the liver and surrounding structures.
- Jaundice: If the cysts obstruct the bile ducts, it can lead to the buildup of bile in the liver, resulting in jaundice (yellowing of the skin and eyes). This condition may be accompanied by dark urine and pale stools.
- Nausea and Vomiting: As cysts enlarge, they can interfere with the digestive system, leading to nausea, vomiting, and a general feeling of discomfort.
- Fatigue and Weakness: Chronic fatigue and weakness may develop as the liver function becomes impaired due to the pressure of the cysts on the liver or as a result of infection.
- Palpable Mass: In some cases, if the cyst is large enough, it may be palpable during a physical exam. A healthcare provider may be able to feel the mass in the upper abdomen.
- Fever and Infection: If the cyst ruptures or becomes infected, it can cause systemic symptoms such as fever, chills, and general malaise. A ruptured cyst can lead to peritonitis or anaphylactic shock, both of which are potentially life-threatening.
Complications of Liver Echinococcal Cysts
If left untreated, liver echinococcal cysts can cause a variety of complications, including:
- Cyst Rupture: A ruptured cyst can release the parasite’s larvae into the surrounding abdominal cavity. This can cause severe allergic reactions such as anaphylactic shock. The rupture can also result in peritonitis (infection of the abdominal lining), which can be fatal without prompt treatment.
- Liver Dysfunction: Large cysts can lead to liver dysfunction, as they obstruct the normal flow of bile or cause pressure on liver tissue. This can lead to jaundice, cirrhosis, and even liver failure in severe cases.
- Metastasis to Other Organs: Though rare, cysts can metastasize to other organs such as the lungs, kidneys, and brain, leading to the formation of new cysts in these organs. This can complicate treatment and worsen the prognosis.
- Biliary Obstruction: The cysts can press on the bile ducts, leading to bile flow obstruction. This can cause cholangitis, a serious inflammation of the bile ducts, or even lead to secondary liver infections.
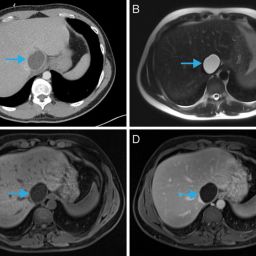
Diagnosing Liver Echinococcal Cysts
Given the slow development and nonspecific nature of the symptoms, diagnosing liver echinococcal cysts can be difficult. However, the following diagnostic techniques are commonly used:
- Ultrasound: Ultrasound imaging is the most common tool for detecting echinococcal cysts. It can identify the presence of cysts, their size, and their location within the liver.
- CT Scan (Computed Tomography): CT scans offer a more detailed view of the cysts and can help differentiate echinococcal cysts from other types of liver lesions. They are also useful for assessing complications such as cyst rupture.
- MRI (Magnetic Resonance Imaging): MRI can provide detailed imaging, particularly in cases where the cysts are complex or when a distinction needs to be made between echinococcal cysts and other liver conditions.
- Serological Tests: Blood tests can detect specific antibodies against Echinococcus, which are present when an individual is infected. These tests can help confirm the diagnosis, but false positives may occur in some cases.
- Biopsy: A biopsy may be performed in some cases to collect tissue from the cyst for microscopic examination to confirm the presence of Echinococcus larvae.
Treatment of Liver Echinococcal Cysts
Treatment of liver echinococcosis depends on several factors, including the size, location, and stage of the cyst, as well as the patient’s overall health. The main treatment options include:
- Surgery: Surgical removal of the cysts is the most effective treatment option for liver echinococcosis. This can be done through traditional open surgery or minimally invasive procedures, such as laparoscopy.
- Percutaneous Aspiration: In cases where surgery is not feasible, percutaneous aspiration may be used. This involves using a needle to drain the cyst and inject a sclerosing agent to kill the larvae.
- Anthelmintic Medications: Drugs like albendazole or mebendazole are used to kill the parasite and prevent further growth of cysts. These medications are often used in conjunction with surgery or when surgery is not an option.
- Liver Transplantation: In cases of extensive liver damage or when other treatments fail, a liver transplant may be necessary.
Prevention of Liver Echinococcal Cysts
Prevention of echinococcosis relies on improving hygiene and reducing exposure to Echinococcus eggs. Some key preventive measures include:
- Proper Hygiene Practices: Regular handwashing, especially after handling animals or soil, is essential to prevent infection. It is also important to wash fruits and vegetables thoroughly.
- De-worming of Dogs: De-worming programs for dogs, especially those that are used in livestock farming, can significantly reduce the spread of Echinococcus.
- Safe Handling of Meat: Properly cooking meat and ensuring that livestock are free from Echinococcus can reduce the likelihood of transmission.
- Environmental Control: Limiting contamination of food and water sources in areas at high risk for echinococcosis is crucial to preventing infection.