1. The Role of the Bile Ducts and Liver Function
Before diving into the specifics of bile duct stricture and its impact on liver function, it is important to understand the essential roles that bile ducts and the liver play in digestion and overall health.
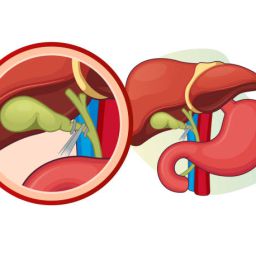
The Bile Duct System:
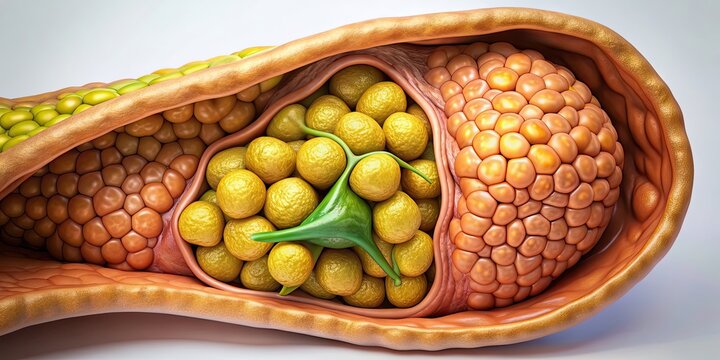
The bile duct system comprises a network of tubes that transport bile from the liver and gallbladder to the small intestine. Bile, a yellow-green fluid produced by the liver, contains substances that help break down fats, absorb fat-soluble vitamins, and eliminate waste products such as bilirubin.
Bile is stored in the gallbladder until it is needed for digestion. When you consume food, especially fatty foods, the gallbladder contracts and releases bile into the small intestine through the bile ducts. This bile helps emulsify fats, making it easier for the body to digest and absorb them.
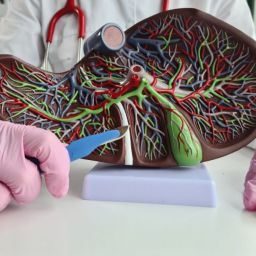
Liver Function:
The liver performs numerous essential functions, including detoxifying harmful substances, storing glycogen for energy, producing proteins necessary for blood clotting, and metabolizing nutrients. One of its most important tasks is the production of bile, which is crucial for digestion and the removal of waste products. Bile is composed of water, electrolytes, bile salts, cholesterol, phospholipids, and bilirubin, which the liver excretes into the bile ducts.
When bile flow is obstructed, it can lead to the accumulation of waste products in the liver, disrupting liver function and causing a variety of symptoms and complications.
2. How Bile Duct Stricture Affects Liver Function
When bile duct stricture occurs, the narrowed or blocked bile ducts prevent bile from flowing freely from the liver to the small intestine. This disruption can lead to several adverse effects on liver function:
A. Cholestasis and Jaundice

Cholestasis refers to the reduction or stoppage of bile flow. When bile cannot flow properly through the bile ducts due to a stricture, it backs up in the liver. This condition is known as intrahepatic cholestasis, and it leads to the accumulation of bile components, such as bilirubin.
Bilirubin is a byproduct of red blood cell breakdown, and when it builds up in the liver and bloodstream, it causes the yellowing of the skin and eyes, a condition known as jaundice. Jaundice is one of the hallmark symptoms of bile duct stricture, and its severity depends on the extent of bile duct obstruction and the liver’s ability to process the bilirubin.
B. Elevated Liver Enzymes
When bile ducts are narrowed or blocked, bile cannot effectively reach the small intestine. As a result, liver cells may become damaged, leading to an increase in liver enzyme levels. These enzymes, such as alanine aminotransferase (ALT), aspartate aminotransferase (AST), and alkaline phosphatase (ALP), are released into the bloodstream when liver cells are damaged or inflamed.
Elevated liver enzymes are often detected through blood tests and are one of the key indicators of liver dysfunction related to bile duct obstruction. Chronic elevation of liver enzymes can indicate ongoing liver damage and may lead to liver cirrhosis if left untreated.
C. Impaired Digestion and Nutrient Absorption
Bile is essential for the digestion and absorption of fats and fat-soluble vitamins (A, D, E, and K). When bile flow is obstructed due to a stricture, the digestive process is significantly impacted. Fats cannot be properly emulsified, leading to steatorrhea, which is the presence of undigested fat in the stool.
In addition, the absorption of essential vitamins is hindered, leading to potential deficiencies in vitamins A, D, E, and K. These deficiencies can have serious consequences on various body functions, including vision, bone health, immune function, and blood clotting.
D. Risk of Liver Damage and Cirrhosis
If bile duct stricture is not diagnosed or treated early, the prolonged build-up of bile in the liver can cause damage to liver cells. Over time, this can lead to fibrosis (scarring of liver tissue). As the fibrosis progresses, it may result in cirrhosis, a condition characterized by severe liver scarring that impairs liver function.
Cirrhosis can lead to complications such as liver failure, portal hypertension, varices (enlarged veins), and liver cancer. The relationship between bile duct obstruction and cirrhosis highlights the importance of early diagnosis and effective treatment to prevent irreversible liver damage.
3. Causes of Bile Duct Stricture and Its Impact on Liver Function
Bile duct strictures can be caused by a variety of factors, each of which can impact liver function differently. The most common causes of bile duct stricture include:

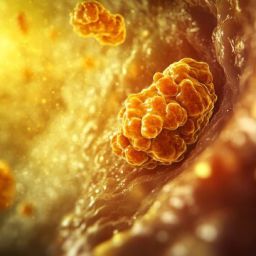
A. Gallstones
Gallstones are hardened deposits that form in the gallbladder and can block the bile ducts. When gallstones migrate from the gallbladder into the bile ducts, they can cause bile duct obstruction. The resulting blockage can lead to increased pressure within the bile ducts, inflammation, and narrowing of the bile ducts over time. This type of obstruction can lead to cholestasis, jaundice, and liver enzyme abnormalities.
B. Inflammatory Conditions
Primary Sclerosing Cholangitis (PSC) is a chronic, progressive disease that causes inflammation and scarring of the bile ducts. It is often associated with other inflammatory conditions, such as inflammatory bowel disease (IBD). PSC can cause gradual bile duct stricture formation, which leads to bile flow obstruction and liver damage.
Chronic cholangitis, an inflammation of the bile ducts, can also lead to scarring and narrowing, contributing to bile duct strictures. This can result in repeated infections and liver dysfunction.
C. Tumors and Cancer
Tumors in or around the bile ducts can obstruct bile flow, leading to bile duct stricture and impacting liver function. Cholangiocarcinoma, or bile duct cancer, is one of the most common cancers that can cause bile duct obstruction. Pancreatic cancer can also compress the bile ducts, leading to stricture formation. Cancer-related strictures often result in more severe liver damage, as tumors can cause more extensive obstruction and compromise liver function more quickly.
D. Surgical and Post-Surgical Complications
Surgical procedures, particularly those involving the liver or gallbladder, can inadvertently cause damage to the bile ducts, leading to strictures. For example, bile duct injury during a cholecystectomy (gallbladder removal surgery) can result in the formation of strictures that impair bile flow and disrupt liver function.
E. Autoimmune Diseases
Autoimmune diseases such as autoimmune hepatitis and IgG4-related disease can cause inflammation and fibrosis of the bile ducts, resulting in strictures. In these cases, the immune system attacks the bile ducts, leading to scarring and impaired bile flow.
4. Diagnosing Bile Duct Stricture and Liver Dysfunction
The diagnosis of bile duct stricture and its impact on liver function typically involves a combination of clinical evaluation, imaging studies, and laboratory tests:
A. Blood Tests
Blood tests are essential in assessing liver function and detecting liver damage. Key indicators include liver enzymes (ALT, AST, ALP), bilirubin levels, and prothrombin time (which measures blood clotting function).
B. Imaging Studies
- Ultrasound: A common first-line imaging technique to assess bile duct dilation and liver abnormalities.
- Magnetic Resonance Cholangiopancreatography (MRCP): A non-invasive imaging technique that provides detailed views of the bile ducts and helps identify strictures.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): A procedure that uses a flexible endoscope to view the bile ducts directly and can help treat strictures by placing stents or performing balloon dilation.
C. Biopsy
In cases where cancer or another serious condition is suspected, a biopsy may be performed to obtain tissue samples for analysis.
5. Treatment of Bile Duct Stricture and Liver Protection
Treating bile duct stricture involves addressing the underlying cause of the stricture, relieving bile flow obstruction, and preventing further liver damage. Treatment options include:
- Endoscopic Stent Placement: A stent can be placed in the bile duct to relieve the obstruction and restore bile flow.
- Balloon Dilation: A procedure where a balloon is used to widen the narrowed bile duct.
- Surgical Repair: In severe cases, surgery may be required to bypass the obstructed bile duct or reconstruct the bile ducts.
- Liver Transplantation: For patients with advanced liver disease due to chronic bile duct stricture, a liver transplant may be necessary.
Bile duct stricture is a serious condition that can disrupt liver function and lead to a variety of complications. The relationship between bile duct stricture and liver function is closely linked, as the inability to properly excrete bile can lead to jaundice, impaired digestion, and, in severe cases, liver failure. Early diagnosis and effective treatment are critical to managing this condition and protecting liver health. By understanding the connection between bile duct stricture and liver function, patients and healthcare providers can work together to prevent long-term liver damage and improve overall health outcomes.