Diverticulitis and Its Impact on Digestion
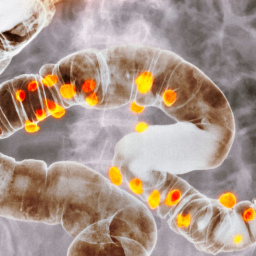
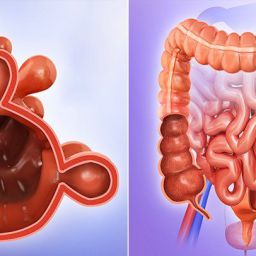
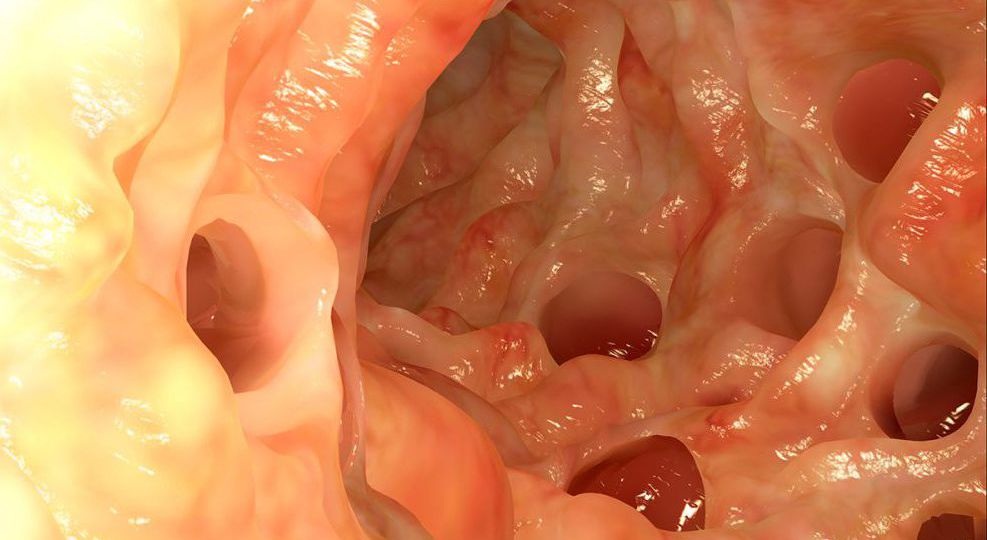
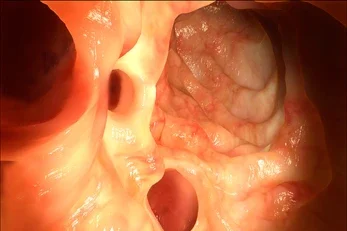
Diverticulitis occurs when diverticula, which are small, bulging sacs that form in the colon wall, become inflamed or infected. These pouches are common in people over the age of 40 and may not cause symptoms until they become inflamed. The inflammation or infection can result in severe abdominal pain, typically on the left side, along with other symptoms such as nausea, vomiting, fever, and changes in bowel movements.
The colon plays a crucial role in digestion, and any disruption to its normal functioning can cause discomfort. Inflammation in the colon can slow down digestion, causing the muscles in the colon to spasm, which leads to bloating, pain, and difficulty passing stool.
A well-balanced diet that includes the right kinds of food can help reduce the strain on the digestive system, particularly during flare-ups of diverticulitis. It’s important to avoid certain foods that can worsen inflammation, cause irritation, or lead to complications such as infection or obstruction.
Foods to Avoid During Diverticulitis Flare-ups
During an acute diverticulitis flare-up, the digestive system is in a heightened state of inflammation. Therefore, it’s essential to avoid foods that can further irritate the colon, increase gas production, or lead to obstruction. Some of the most common foods that should be avoided during this period include:
1. High-Fiber Foods
While fiber is an essential part of a healthy diet, during an active flare-up of diverticulitis, high-fiber foods can be difficult to digest and may worsen symptoms. High-fiber foods can increase bowel movement frequency and cause more bloating, cramping, and discomfort.
Foods to avoid:
- Whole grains (e.g., whole wheat bread, brown rice, quinoa)
- Legumes (e.g., beans, lentils, chickpeas)
- Cruciferous vegetables (e.g., broccoli, cauliflower, Brussels sprouts)
- Certain fruits (e.g., apples, pears, and berries with seeds or skins)
- Nuts and seeds (e.g., sunflower seeds, flaxseeds, almonds)
These foods can be particularly challenging for people with diverticulitis because they are high in insoluble fiber, which can irritate the inflamed colon and cause increased gas production.
2. Tough Meats and Processed Foods
Tough cuts of meat and processed foods can be difficult for the digestive system to break down, especially when the colon is inflamed. These foods can also increase the risk of constipation, which can exacerbate diverticulitis symptoms.
Foods to avoid:
- Red meats (e.g., beef, pork)
- Processed meats (e.g., sausages, hot dogs, bacon)
- Dried meats (e.g., jerky)
Lean proteins such as skinless chicken or fish are generally easier to digest and are preferable options during a flare-up. It’s also important to avoid fatty cuts of meat as they can cause gastrointestinal discomfort.
3. Fried and Greasy Foods
Fried and greasy foods are high in fat, which can slow down digestion and lead to bloating and discomfort. Inflammation in the colon can already make digestion difficult, and these types of foods can worsen symptoms such as nausea, pain, and bloating.
Foods to avoid:
- Fried foods (e.g., French fries, fried chicken, fried fish)
- Fast food (e.g., hamburgers, pizza, fried snacks)
- Heavy sauces and gravies (especially those made with butter or cream)
During an acute flare-up, it’s best to avoid greasy, fried foods and instead opt for foods that are steamed, baked, or grilled to minimize digestive strain.
4. Dairy Products
Dairy products can be problematic for some people with diverticulitis, especially during a flare-up. Lactose intolerance, which is common in individuals with gastrointestinal conditions, can cause bloating, gas, diarrhea, and abdominal pain. Even if you do not have lactose intolerance, dairy products can be harder to digest when your digestive system is inflamed.
Foods to avoid:
- Milk
- Cheese
- Cream-based sauces and soups
- Ice cream
If you suspect dairy is aggravating your symptoms, consider reducing your intake or choosing lactose-free alternatives. Non-dairy milks such as almond or oat milk can be beneficial substitutes.
5. Caffeinated and Carbonated Beverages
Caffeine and carbonated beverages can both irritate the digestive system, causing symptoms like acid reflux, bloating, and discomfort. Caffeine is a stimulant, and it can lead to increased bowel movements, which is not ideal during a flare-up when the colon is already inflamed. Carbonated drinks, on the other hand, can lead to excess gas production and bloating.

Drinks to avoid:
- Coffee
- Sodas
- Energy drinks
- Alcoholic beverages
It is best to drink plenty of water and opt for herbal teas such as ginger or chamomile tea, which can help soothe the digestive system.
6. Spicy and Irritating Foods
Spicy foods can cause irritation and exacerbate symptoms in individuals with diverticulitis. Spices such as chili, curry, and hot sauce can irritate the stomach lining and cause gastrointestinal discomfort. Additionally, acidic foods can also increase inflammation and trigger symptoms such as acid reflux, heartburn, or stomach cramps.
Foods to avoid:
- Hot peppers
- Curry
- Spicy condiments and sauces
Instead of spicy foods, it’s better to stick to mild, bland foods that are easier on the digestive system, such as plain rice, boiled potatoes, or grilled vegetables.
7. Artificial Sweeteners
Artificial sweeteners, found in sugar-free gum, candies, and soft drinks, can irritate the digestive tract and cause bloating, diarrhea, and discomfort. These sweeteners are not fully absorbed by the body and can ferment in the colon, leading to excess gas production.
Sweeteners to avoid:
- Aspartame
- Sorbitol
- Sucralose
It’s advisable to choose natural sweeteners such as honey or maple syrup, but it’s important to use these in moderation.
Transitioning Back to a Normal Diet
After the acute symptoms of diverticulitis have been treated and inflammation has subsided, a healthcare provider may suggest gradually transitioning to a normal diet, which includes more fiber. A high-fiber diet helps keep the colon healthy and prevents future flare-ups. However, it’s essential to reintroduce fiber slowly to avoid further irritation.
Foods to Include in Your Post-Diverticulitis Diet:
- Low-fiber options (during the acute phase): White bread, plain pasta, white rice, cooked vegetables without skins.
- Gradual fiber reintroduction: Gradually add high-fiber foods, including fruits, vegetables, whole grains, and legumes, to prevent overwhelming the digestive system.
Diverticulitis is a serious condition that requires careful management, especially during flare-ups. One of the most effective ways to support your recovery and reduce symptoms is by modifying your diet. Avoiding high-fiber foods, tough meats, fried foods, dairy products, carbonated beverages, and irritants such as spicy foods and alcohol can help reduce inflammation and prevent further complications.
As you recover, a gradual transition back to a high-fiber diet can promote long-term digestive health and prevent future flare-ups. It’s always recommended to work with a healthcare provider or nutritionist to create a personalized diet plan based on your individual needs.