Understanding Focal Nodular Hyperplasia (FNH)
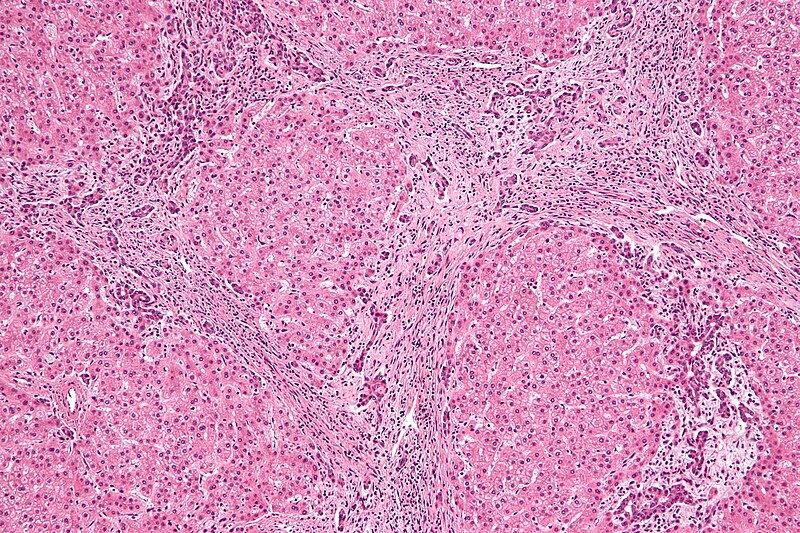
Before delving into the issue of size and its implications, it’s essential to have a clear understanding of what FNH is. Focal Nodular Hyperplasia refers to an abnormal growth of liver tissue that results from a vascular anomaly. The lesion typically consists of a central scar surrounded by normal liver tissue that has undergone hyperplasia (excessive growth). While it is most commonly found in women between the ages of 20 and 50, it can occur in men as well.
FNH is generally asymptomatic and typically does not require treatment. The majority of cases are diagnosed incidentally through imaging tests, such as ultrasound, CT scans, or MRIs, which are often performed for other reasons. Due to the benign nature of FNH, most individuals live normal, healthy lives without the need for medical intervention.
However, as with any medical condition, there are situations in which the size or progression of FNH might warrant concern and require further evaluation or treatment.
When Does the Size of FNH Become a Concern?
FNH lesions are typically small, measuring a few centimeters in diameter. In most cases, these lesions remain stable in size over time and do not cause symptoms. However, in some cases, the size of the lesion may become a factor in determining whether further action is needed. The following factors should be considered when assessing whether the size of an FNH lesion is a cause for concern:
1. Size of the Lesion
The size of an FNH lesion is one of the key factors that may raise concern. Generally, smaller lesions that are less than 5 cm in diameter are considered to be relatively harmless and do not require treatment. However, if an FNH lesion grows to a significant size (typically greater than 5 cm), it may begin to cause symptoms or complications.
In some rare cases, very large FNH lesions (greater than 10 cm) can lead to complications such as:

- Abdominal pain or discomfort: Larger lesions may press on nearby organs or structures, leading to discomfort or pain in the abdomen.
- Liver dysfunction: In some cases, a very large lesion may interfere with the liver’s ability to function properly, leading to problems such as jaundice or altered liver enzyme levels.
- Bleeding: FNH lesions can have abnormal blood vessels, and large lesions might be at an increased risk of bleeding, although this is a rare complication.
While the majority of FNH lesions remain stable and do not cause significant problems, large lesions may require closer monitoring and, in some cases, intervention.
2. Symptoms Associated with FNH Size
While FNH is typically asymptomatic, the size of the lesion can influence whether symptoms develop. Large FNH lesions may compress nearby structures, including the bile ducts, gallbladder, or blood vessels. This compression can result in symptoms such as:
- Abdominal pain or fullness: A large lesion might cause a sensation of fullness or discomfort in the upper abdomen, especially after eating.
- Jaundice: If the lesion presses against the bile ducts and obstructs bile flow, it may lead to jaundice, which is characterized by the yellowing of the skin and eyes.
- Nausea or vomiting: Larger lesions may cause nausea or vomiting if they affect the liver’s ability to function properly or cause irritation in the abdominal cavity.
- Hepatomegaly (Enlarged Liver): In rare cases, large FNH lesions may lead to hepatomegaly, which is the abnormal enlargement of the liver. Hepatomegaly can be detected during a physical examination.
If a patient experiences any of these symptoms and the size of the FNH lesion is found to be large, further evaluation and possibly treatment may be necessary.
3. Growth and Change in Size Over Time
In most cases, FNH lesions remain stable over time and do not change in size. However, if a lesion begins to grow or if there is a rapid increase in its size, this could raise concerns. Rapid growth could be indicative of an underlying issue, such as:

- Atypical growth patterns: While FNH is generally stable, in some cases, lesions may grow more rapidly than expected. This could be due to other factors, such as hormonal changes or an undiagnosed vascular anomaly.
- Misdiagnosis or other liver conditions: In some cases, an FNH lesion might be misdiagnosed, and the lesion could actually be a malignant tumor or another type of liver pathology that warrants more aggressive treatment.
If a lesion begins to grow rapidly, follow-up imaging tests should be scheduled to assess its size and appearance. It is important to differentiate between benign growth and the possibility of malignancy.
4. Location of the Lesion
In addition to the size of the lesion, its location within the liver can also play a role in determining whether the size is concerning. For instance, FNH lesions located in areas that are more likely to affect surrounding structures, such as the bile ducts or major blood vessels, may be of greater concern if they become large.
Lesions located near the edge of the liver or in areas that are difficult to monitor might also require closer attention. For example, lesions near the hepatic veins or portal vein may lead to complications related to blood flow, whereas lesions near the bile ducts might affect bile drainage and cause jaundice.
5. Risk of Malignancy and Misdiagnosis
Although FNH is a benign condition, it is important to distinguish it from other liver lesions that could be cancerous or cause serious complications. In rare cases, a lesion initially thought to be FNH may turn out to be another condition, such as:
- Hepatic Adenomas: These are also benign liver lesions but are associated with a higher risk of bleeding and, in rare cases, malignant transformation.
- Hepatocellular Carcinoma (HCC): HCC is a type of liver cancer that may resemble FNH on imaging tests. If a lesion grows rapidly or presents with other suspicious features, it is essential to conduct further tests to rule out malignancy.
- Metastatic liver cancer: FNH lesions are often found incidentally and can be misdiagnosed as metastases from other cancers. It is essential to monitor the lesion’s growth pattern and ensure accurate diagnosis.
In cases where there is any doubt about the diagnosis, further diagnostic testing such as a biopsy, advanced imaging, or angiography may be necessary to clarify the nature of the lesion.
6. Treatment Considerations Based on Size
In most cases, treatment for FNH is not necessary, as the lesion is benign and asymptomatic. However, for larger lesions or those that cause significant symptoms, treatment options may be considered. These could include:
- Observation and Monitoring: For most patients, monitoring the lesion with regular imaging tests is sufficient. A lesion that is stable in size and not causing symptoms typically does not require intervention.
- Surgical Intervention: In cases where the lesion causes severe symptoms or complications, surgical removal may be considered. This is typically reserved for large lesions that lead to pain, liver dysfunction, or the risk of bleeding.
- Hormonal Therapy Adjustment: Since FNH is more common in women, particularly those taking oral contraceptives or undergoing hormonal treatments, adjusting or discontinuing these therapies may help reduce the risk of lesion growth.
The size of an FNH lesion is an important factor in determining whether it poses a risk to health. In most cases, small lesions are benign and do not require treatment. However, larger lesions may cause symptoms such as abdominal pain, liver dysfunction, or jaundice, and these should be monitored closely. Additionally, rapid growth or changes in the size of the lesion may warrant further investigation to rule out other potential liver conditions.
Ultimately, the decision to intervene in cases of FNH should be made by a healthcare provider based on the individual’s symptoms, the size and growth of the lesion, and other diagnostic findings. Regular follow-up and imaging are crucial in managing FNH and ensuring that any potential complications are identified early.

