1. Overview of Soft Tissue Cancer
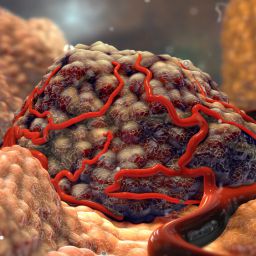
A. What is Soft Tissue Cancer?
Soft tissue cancers are a diverse group of malignancies that arise from the body’s connective tissues. Soft tissue sarcomas can develop in any part of the body, though they are most commonly found in the arms, legs, abdomen, and retroperitoneum. These cancers can be classified into several subtypes based on the type of tissue involved, including:
- Liposarcoma (fat tissue)
- Leiomyosarcoma (smooth muscle)
- Rhabdomyosarcoma (skeletal muscle)
- Synovial sarcoma (joint lining)
- Angiosarcoma (blood vessels)
Soft tissue sarcomas represent less than 1% of all cancers, but they are known for their aggressive nature, tendency to recur locally, and potential to metastasize, especially to the lungs. Diagnosis is typically made through imaging studies (such as CT, MRI, and PET scans) and biopsy.
B. Treatment of Soft Tissue Cancer
Treatment for soft tissue sarcoma generally involves a multimodal approach, combining surgery, radiation therapy, and chemotherapy. The goal of treatment is to remove or shrink the tumor, prevent recurrence, and improve survival. The choice of treatment depends on several factors, such as:

- Tumor size and location
- Histologic subtype
- Tumor grade (how aggressive it is)
- Stage of the cancer (localized vs. metastatic)
- Patient’s overall health and comorbidities
Surgical intervention is the primary treatment for most soft tissue sarcomas, but the decision to perform surgery and the type of surgery performed depends on a number of clinical considerations, which will be discussed in detail below.
2. Factors That Influence the Decision to Perform Surgery
The decision to proceed with surgery as a treatment option for soft tissue sarcoma is based on several key factors, including tumor characteristics, the patient’s health, and the likelihood of achieving clear surgical margins (ensuring all cancerous tissue is removed).
A. Tumor Size and Location
The size and location of the soft tissue tumor are crucial factors in determining whether surgery is appropriate. Small tumors that are confined to a single area are generally more amenable to surgical removal. In contrast, larger tumors or those located near critical structures (e.g., major blood vessels, nerves, or organs) may require more complex surgical approaches, such as limb-sparing surgery or reconstructive surgery.
For tumors that are located deep within the body (e.g., in the retroperitoneum or pelvis), surgical intervention may be more challenging due to the proximity of vital organs. In these cases, the surgeon may need to balance the need for complete tumor resection with the preservation of important structures.
B. Tumor Grade and Histological Subtype
Soft tissue sarcomas vary in terms of their histological subtypes, and some types are more aggressive than others. The tumor grade, which refers to how abnormal the cancer cells look under the microscope, is another critical factor. Low-grade sarcomas tend to grow more slowly and are less likely to spread, whereas high-grade sarcomas are more aggressive and have a higher potential for metastasis.
For high-grade tumors, surgery is often recommended as the primary treatment, but it may be combined with other therapies, such as radiation or chemotherapy, to reduce the risk of recurrence. Conversely, for low-grade tumors, surgery may be sufficient on its own, though close monitoring is necessary.
C. Clear Surgical Margins
One of the most important considerations in soft tissue cancer surgery is the ability to achieve clear surgical margins, meaning that the tumor is completely removed along with a surrounding buffer of healthy tissue. If the tumor cannot be completely removed due to its size, location, or other factors, the risk of recurrence is higher.
In some cases, preoperative radiation therapy may be used to shrink the tumor before surgery, making it easier to remove it with clear margins. Similarly, if the tumor is located in a challenging area, the surgical team may employ advanced techniques, such as intraoperative imaging, to ensure that all cancerous tissue is excised.
D. Metastatic Disease and Surgery
Soft tissue sarcomas can metastasize to distant organs, particularly the lungs. When the disease has spread, the role of surgery becomes more complex. Surgery may be considered for isolated metastases, especially if they are limited to a single site (e.g., a solitary lung metastasis). However, if the cancer has spread extensively, surgery may not be the best option, and other treatments, such as chemotherapy or targeted therapies, may be recommended.
In cases of metastatic soft tissue sarcoma, the goal of surgery is often to improve the patient’s quality of life, relieve symptoms, or reduce tumor burden, rather than to cure the disease.
E. Patient’s Overall Health and Age
The patient’s overall health, age, and ability to tolerate surgery are significant factors in determining whether surgery is the best treatment option. Surgery for soft tissue sarcoma can be extensive and may involve long recovery times. For older patients or those with significant comorbidities (e.g., heart disease, diabetes), surgery may be riskier and less likely to result in a favorable outcome.
In these cases, a multidisciplinary team of oncologists, surgeons, and other healthcare providers will carefully assess the risks and benefits of surgery, taking into account the patient’s quality of life and personal preferences.
3. Types of Surgical Procedures for Soft Tissue Cancer
Several surgical approaches may be used in the treatment of soft tissue sarcomas, depending on the tumor’s location, size, and other factors.

A. Wide Local Excision (WLE)
Wide local excision is the standard surgical procedure for removing soft tissue sarcomas. This procedure involves removing the tumor along with a margin of surrounding healthy tissue to ensure that no cancer cells are left behind. WLE is typically the preferred method for tumors located in accessible areas and those that can be removed without affecting vital structures.
B. Limb-Sparing Surgery
Limb-sparing surgery is often employed for soft tissue sarcomas located in the limbs. This procedure aims to remove the tumor while preserving as much of the limb’s function as possible. In some cases, reconstructive surgery may be necessary to restore function or appearance.
C. Amputation
In some cases, particularly for tumors located in the extremities where complete removal with clear margins is not possible, amputation may be considered. While amputation is generally reserved for more advanced cases, it may be the best option for ensuring complete removal of the tumor and preventing recurrence.
D. Reconstructive Surgery
In cases where extensive tissue removal is necessary, reconstructive surgery may be required to restore the appearance and function of the affected area. This may involve skin grafts, muscle flaps, or prosthetic devices, depending on the tumor’s location and the type of surgery performed.
E. Lymph Node Dissection
In some cases, if there is a concern that the cancer has spread to the lymph nodes, a lymph node dissection may be performed. This involves removing nearby lymph nodes to check for metastasis.
4. Postoperative Care and Rehabilitation
After surgery for soft tissue sarcoma, patients require careful monitoring and rehabilitation. The recovery process can be lengthy, especially for more extensive surgeries, and may involve physical therapy to regain strength and function in the affected area. Pain management and wound care are also critical components of postoperative care.
In some cases, additional treatments, such as radiation therapy or chemotherapy, may be necessary after surgery to reduce the risk of recurrence. Regular follow-up appointments and imaging studies are essential for detecting any signs of recurrence or metastasis.
Surgical intervention is a key component of treatment for soft tissue cancer, and it remains the preferred approach for most patients. However, the decision to undergo surgery depends on several factors, including the size, location, and grade of the tumor, as well as the patient’s overall health and the presence of metastases. In many cases, surgery is combined with other treatments, such as radiation or chemotherapy, to improve outcomes and reduce the risk of recurrence.
The decision to pursue surgical intervention should always be made by a multidisciplinary team of oncologists, surgeons, and other healthcare professionals, who can assess the unique characteristics of the patient’s case and determine the most appropriate course of action. By considering all relevant factors, patients can receive personalized care that maximizes their chances of a successful outcome and improves their quality of life.