The Connection Between Family History and Thyroid Cancer Risk
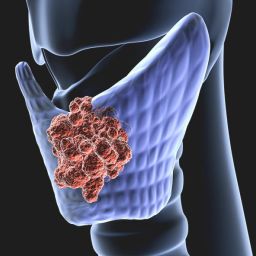
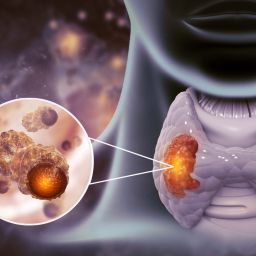
The thyroid is a butterfly-shaped gland located in the neck that plays a crucial role in regulating metabolism and producing hormones that influence various bodily functions. Thyroid cancer occurs when abnormal cells begin to grow uncontrollably within the thyroid gland. While most thyroid cancer cases are not hereditary, there are certain genetic factors that increase the likelihood of developing this cancer.
A family history of thyroid cancer, particularly in first-degree relatives (parents, siblings, children), can significantly elevate the risk of thyroid cancer. Inherited genetic mutations, such as those associated with familial medullary thyroid cancer (FMTC) and multiple endocrine neoplasia (MEN), are linked to thyroid cancer. These conditions may predispose individuals to developing thyroid cancer at an earlier age or in multiple members of a family.
Why Early Check-Ups Are Important
When thyroid cancer is detected early, it is often more treatable and has a better prognosis. However, many types of thyroid cancer grow slowly and may not cause symptoms until they are more advanced. This is one of the main reasons why regular check-ups are critical for those with a family history of thyroid cancer. Early detection allows for more effective treatment, which can include surgery, radiation, and/or hormone therapy.
For individuals with a family history, the importance of early screening becomes even more crucial. The risk of developing thyroid cancer increases, and screening can help identify potential issues before they become problematic. Understanding when to begin check-ups, what kind of tests are recommended, and how often these check-ups should occur can help individuals navigate the early detection process.
When Should the First Check-Up Take Place?
For individuals with a family history of thyroid cancer, it is essential to take proactive steps toward monitoring their health. The timing of the first check-up is influenced by several factors, including age, family history specifics, and any symptoms that might arise. However, general guidelines can help determine the most appropriate time for an initial check-up.
1. Early Detection Guidelines Based on Age
For individuals without any family history, the risk of developing thyroid cancer is relatively low. However, family members of someone with thyroid cancer may need to begin their screenings at an earlier age.
Family History of Thyroid Cancer and Screening Recommendations:
- Children and Adolescents (under 18 years): For children and adolescents with a family history of thyroid cancer or genetic conditions like MEN2 or FMTC, it is recommended that screenings begin early, often during adolescence. A pediatrician or endocrinologist will provide guidance based on the specific risks in the family.
- Young Adults (18-40 years): If you have a family history of thyroid cancer, it is generally recommended to begin regular check-ups by the time you reach adulthood. While thyroid cancer is rare in young adults, starting early is beneficial for peace of mind and early detection if any signs or symptoms occur. A check-up every 1-2 years may be advised during this stage.
- Adults Over 40 (40-60 years): As individuals approach middle age, the risk of thyroid cancer increases slightly, particularly if a family history is involved. Adults over 40 with a family history should have a thyroid check-up at least once every year. During this time, it is also essential to monitor any changes in symptoms, such as unexplained neck lumps, difficulty swallowing, or hoarseness, which could indicate thyroid issues.
- Seniors (Over 60 years): For older adults with a family history of thyroid cancer, regular check-ups every year are essential. Thyroid cancer tends to have a more indolent course in older adults, and early detection remains crucial. Screening typically includes a physical exam, ultrasound, and possibly fine-needle aspiration biopsy if necessary.
2. Family History of Genetic Syndromes
Certain genetic conditions increase the likelihood of developing thyroid cancer. If you have a family history of conditions such as Multiple Endocrine Neoplasia Type 2 (MEN2) or Familial Medullary Thyroid Cancer (FMTC), early and frequent screenings are recommended. These genetic conditions are linked to a higher risk of developing thyroid cancer at a younger age.
- MEN2: Individuals with MEN2, a genetic syndrome linked to thyroid cancer, are often advised to undergo genetic counseling and screening beginning in childhood. Screening may include genetic testing for mutations in the RET gene, which are associated with MEN2. Those diagnosed with MEN2 should undergo thyroid monitoring regularly, starting as early as age 5 or 6.
- FMTC: For families with a history of FMTC, the onset of thyroid cancer typically occurs during young adulthood. Early screening with ultrasound and blood tests (e.g., calcitonin levels) should begin in early adolescence to catch any issues early.
3. Regular Monitoring and Physical Exams
A family history of thyroid cancer may warrant more frequent monitoring than what is typically recommended for the general population. Regular physical exams conducted by a healthcare provider should be part of any early detection plan. During these exams, healthcare professionals will assess for common symptoms of thyroid cancer, such as:
- Lumps or nodules in the neck
- Changes in voice or hoarseness
- Difficulty swallowing
- Pain in the throat or neck
If any abnormalities are detected during these exams, additional testing, such as an ultrasound or biopsy, may be ordered. Even in the absence of symptoms, regular check-ups can help monitor for any potential signs of cancer development.
Screening Tests for Thyroid Cancer
Screening for thyroid cancer often begins with non-invasive tests and procedures, such as physical examinations, blood tests, and imaging. The tests selected will depend on the patient’s age, family history, and any symptoms present. Common tests include:
1. Physical Examination
A healthcare provider will examine the neck for any lumps, swelling, or tenderness. If a lump is detected, it may be evaluated further with imaging tests or a biopsy.
2. Thyroid Ultrasound
Ultrasound is a non-invasive imaging technique that helps detect thyroid nodules or abnormalities. If a lump or nodule is found during a physical exam, an ultrasound may be the first step in assessing its characteristics.
3. Fine Needle Aspiration Biopsy
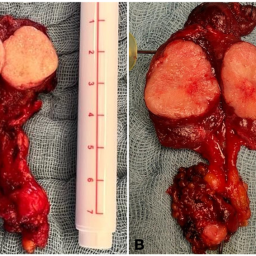
If a nodule appears suspicious on an ultrasound, a fine needle aspiration (FNA) biopsy may be performed. This procedure involves taking a small sample of tissue from the thyroid to examine for cancerous cells.
4. Blood Tests
While thyroid blood tests (e.g., TSH, T4, and T3) are used to assess thyroid function, certain markers, like calcitonin and thyroglobulin, may be monitored in individuals with a family history of thyroid cancer or genetic conditions like MEN2 or FMTC.
Thyroid cancer, while rare, can be particularly concerning for those with a family history of the disease. Early detection is key to improving outcomes, and individuals with a family history should begin screening at an age determined by both their personal and family medical history. Regular check-ups, physical exams, and appropriate imaging tests are vital for identifying potential issues early.
If you have a family history of thyroid cancer or genetic syndromes related to thyroid cancer, it’s important to work closely with your healthcare provider to develop a personalized screening plan. Through vigilance, awareness, and timely check-ups, individuals can significantly reduce their risk of undiagnosed thyroid cancer and improve their overall health outcomes.
Early action can lead to early detection, and early detection can lead to more successful treatment options. Regular screening and self-awareness are key to navigating thyroid cancer prevention in families with a history of this condition.