1. The Stages of Anal Fissures: Acute vs. Chronic
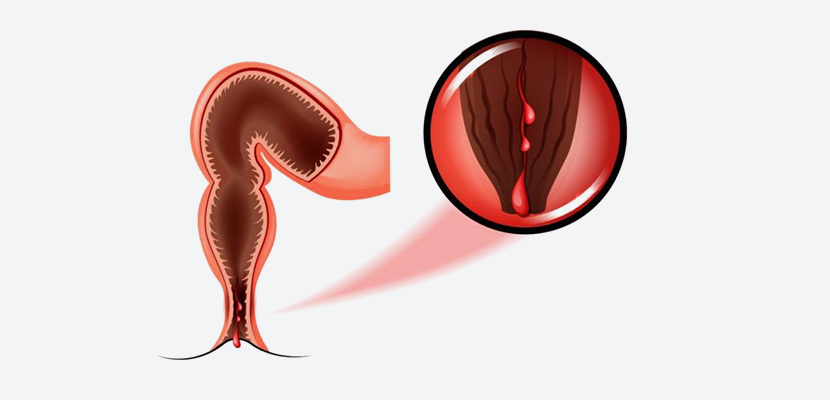
Anal fissures can be classified as either acute or chronic, with the primary distinction being the duration of symptoms and the level of tissue damage.
- Acute Anal Fissures: An acute anal fissure is a new tear in the skin that typically causes sharp pain during or after bowel movements. In these cases, the fissure may heal within a few days to weeks with appropriate treatment, which usually includes increasing fiber intake, using stool softeners, and applying topical medications to relieve pain and inflammation.
- Chronic Anal Fissures: Chronic anal fissures, on the other hand, persist for more than six weeks despite conservative treatment. The prolonged exposure to trauma during bowel movements leads to deeper fissures that may become harder to heal. Over time, the tissue around the fissure may develop scar tissue, making the condition more resistant to non-surgical treatment. Chronic fissures are often accompanied by additional complications, such as anal sphincter spasm, which further impedes healing.
2. Symptoms of Chronic Anal Fissures
The symptoms of chronic anal fissures are typically more severe and persistent than those associated with acute fissures. Common signs include:
- Pain During and After Bowel Movements: This is the hallmark symptom of anal fissures. The pain can be sharp and intense, often lasting for hours after a bowel movement.
- Bleeding: Bright red blood may be noticed on the toilet paper or in the stool.
- Itching or Irritation: The fissure site may itch or feel irritated, leading to further discomfort.
- Visible Tear or Crack: In some cases, a visible tear may be seen at the anus during an examination.
- Fistula Formation: In severe cases, a fistula may develop, creating an abnormal connection between the anal canal and the skin surrounding the anus.
- Sphincter Spasms: In chronic cases, the anal sphincter muscles may spasm, further contributing to pain and impeding healing.
3. When to Consider Surgery for Chronic Anal Fissures
Most acute anal fissures heal on their own with proper care, but chronic fissures may require surgical intervention. Surgery becomes necessary when:
- Conservative Treatments Fail: If dietary changes, stool softeners, topical creams, and other non-surgical treatments do not result in healing after six weeks, surgery may be considered.
- Severe Pain and Discomfort: For patients with chronic pain that significantly impacts their quality of life, surgical intervention may provide relief.
- Development of Anal Sphincter Spasm: Chronic anal fissures often cause spasm of the anal sphincter, which can exacerbate pain and prevent healing. In such cases, surgery may be needed to release the spasm.
- Recurrent Fissures: Some individuals may experience recurrent anal fissures that fail to heal or keep coming back after conservative treatment. Surgery may offer a more permanent solution.
- Fistula Formation: If an anal fistula develops, surgical intervention is often required to treat both the fissure and the fistula.
- Presence of Scar Tissue: Chronic fissures can lead to the development of scar tissue around the tear, which may impair the healing process and require surgical repair.
4. Surgical Options for Chronic Anal Fissures
Several surgical options are available for treating chronic anal fissures, each with its own indications, benefits, and potential risks.
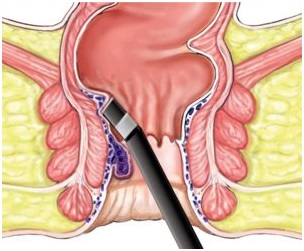
a. Lateral Internal Sphincterotomy (LIS)
Lateral internal sphincterotomy is the most common surgical procedure used to treat chronic anal fissures. The procedure involves making a small incision in the anal sphincter muscle to relax the muscle and reduce spasm. This allows the fissure to heal more effectively by improving blood flow to the area and relieving pressure during bowel movements.
- Benefits: LIS has a high success rate in healing chronic anal fissures and provides significant pain relief. Most patients experience a quick recovery, with minimal discomfort post-surgery.
- Risks: While LIS is generally safe, it carries some risks, such as infection, bleeding, or incontinence. However, the risk of incontinence is relatively low, especially when performed by an experienced surgeon.
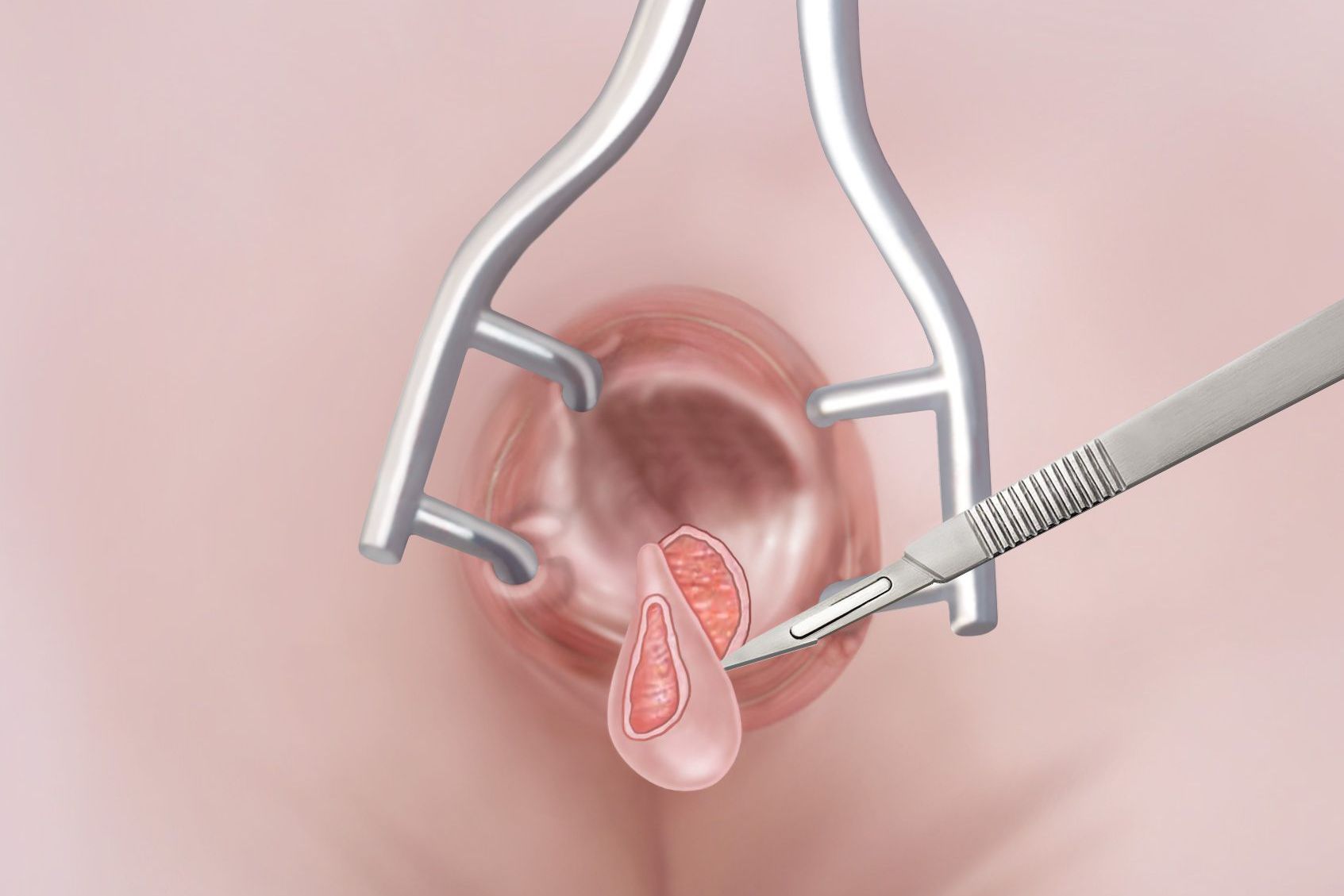
b. Fissurectomy
Fissurectomy involves the surgical removal of the chronic fissure and any surrounding scar tissue. This procedure may be performed in combination with sphincterotomy if the anal sphincter is tight and contributes to the fissure’s persistence.
- Benefits: Fissurectomy can be effective for patients with significant scar tissue or recurrent fissures. It provides an opportunity to remove the damaged tissue and promote healing.
- Risks: As with any surgery, there are risks of infection, bleeding, and complications from anesthesia. Recovery time may also be longer compared to other procedures.
c. Botulinum Toxin (Botox) Injections
Botox injections are a less invasive alternative to surgery. Botox is injected into the anal sphincter to temporarily paralyze the muscle, which helps reduce spasm and allows the fissure to heal.
- Benefits: Botox injections are a quick and minimally invasive procedure, and they can offer pain relief and improve healing without the need for traditional surgery. The procedure has fewer risks and a faster recovery time.
- Risks: The effects of Botox are temporary, and the procedure may need to be repeated. There is also a risk of over-relaxing the anal sphincter, which can lead to incontinence.
d. Advancement Flap Procedure
In cases where the fissure is large or associated with a fistula, an advancement flap procedure may be used. This involves removing the fissure and surrounding tissue and then repositioning a flap of healthy tissue to cover the area, promoting healing.
- Benefits: This procedure is useful for complex fissures or those associated with fistulas. It helps ensure that the area heals without scarring.
- Risks: The risks include infection, wound healing issues, and the possibility of needing additional surgery.
5. Post-Surgical Care and Recovery
After surgery, patients will need to follow specific guidelines to promote healing and avoid complications. These may include:
- Pain Management: Pain relief medications will be prescribed to manage discomfort after surgery.
- Stool Softeners: To prevent constipation and reduce strain on the healing anal area, stool softeners or a high-fiber diet may be recommended.
- Warm Sitz Baths: Soaking in warm water can help soothe the anal area and promote healing.
- Avoiding Strenuous Activity: Patients should avoid heavy lifting and intense physical activity during the recovery period.
- Follow-Up Appointments: Regular follow-up visits with the surgeon are essential to monitor healing progress and detect any complications early.
6. Potential Complications of Surgery
While surgical treatment for chronic anal fissures is often successful, there are potential complications to be aware of:
- Infection: As with any surgery, there is a risk of infection, which can slow down healing and require additional treatment.
- Incontinence: A small percentage of patients may experience temporary or permanent incontinence after sphincterotomy. This is more likely if the sphincter muscle is excessively cut.
- Recurrence of Fissure: In some cases, the fissure may recur despite surgery, especially if underlying factors like constipation or sphincter dysfunction are not addressed.
Chronic anal fissures can be incredibly painful and debilitating, but surgery offers a highly effective solution for many patients when conservative treatments fail. The decision to undergo surgery should be made in consultation with a healthcare provider, considering the severity of the fissure, the patient’s overall health, and the potential risks and benefits of the procedure. With the right treatment plan, most patients can find relief from chronic anal fissures and enjoy a significant improvement in their quality of life.



