1. Immediate Medical Management After Diagnosis
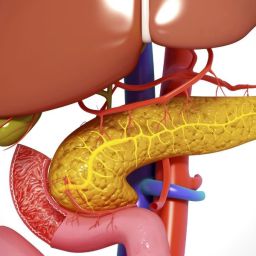
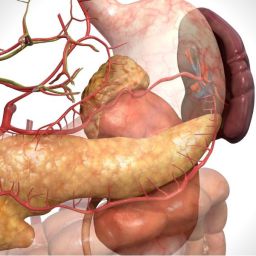
The primary goal of treatment for acute pancreatitis is to reduce inflammation, control symptoms, and prevent complications. Once the diagnosis is confirmed, immediate medical intervention is necessary. This may include the following:
1.1. Hospitalization and Monitoring
Most individuals with acute pancreatitis require hospitalization. The severity of the condition will determine the length of stay. Patients are typically admitted to a hospital for observation, pain management, and supportive care. Close monitoring of vital signs, including blood pressure, heart rate, and respiratory rate, is necessary. Monitoring also includes:
- Blood tests: To check for elevated levels of pancreatic enzymes (amylase and lipase), liver function tests, electrolytes, and kidney function.
- Imaging: An ultrasound or CT scan to assess the extent of pancreatic damage, detect complications like pancreatic necrosis, or rule out other potential causes.
1.2. Fasting the Digestive System
In the early stages of acute pancreatitis, the pancreas needs to rest. This is achieved by keeping the patient NPO (nothing by mouth) for at least 24-48 hours. This helps reduce the secretion of pancreatic enzymes and prevents further irritation to the pancreas. The body is usually hydrated with IV fluids to maintain electrolyte balance.
1.3. Pain Management
Acute pancreatitis often causes intense abdominal pain. Pain relief is a critical part of managing the condition. Analgesics like acetaminophen or stronger opioids (morphine or hydromorphone) may be prescribed depending on the severity of the pain. Pain control is essential to improving the patient’s quality of life and preventing complications such as respiratory issues due to pain-induced immobility.
1.4. Nutritional Support
After the acute phase of pancreatitis, once the symptoms improve, the patient may be allowed to start a clear liquid diet. Gradually, the diet will progress from liquids to solid foods as tolerated. In some cases, where oral feeding is not possible due to severe illness, enteral feeding via a tube may be initiated.
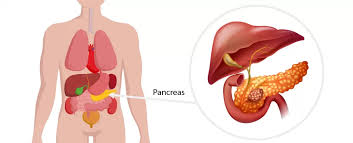
2. Identifying the Underlying Cause
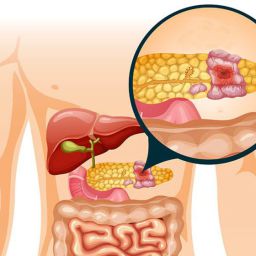
After the diagnosis of acute pancreatitis, it is crucial to determine the underlying cause. Identifying the trigger will help guide treatment decisions and prevent future episodes. The most common causes of acute pancreatitis include:
- Gallstones: The most frequent cause in adults. Gallstones block the bile duct, which can result in inflammation of the pancreas.
- Alcohol consumption: Chronic or excessive alcohol use is a significant risk factor for acute pancreatitis.
- Medications: Certain drugs, including corticosteroids, diuretics, and antibiotics, can induce acute pancreatitis.
- Infections: Viral infections like mumps or coxsackievirus can lead to pancreatic inflammation.
- Trauma or surgery: Trauma to the pancreas, whether from a car accident or medical procedures, can also cause acute pancreatitis.
2.1. Addressing the Cause
- For gallstones: If gallstones are the primary cause, the patient may need a procedure to remove the gallstones, such as an endoscopic retrograde cholangiopancreatography (ERCP) or surgery to remove the gallbladder (cholecystectomy).
- For alcohol use: Patients diagnosed with acute pancreatitis due to alcohol consumption must be advised to avoid alcohol entirely. Detoxification and counseling may also be necessary.
- For medications: If medications are identified as the cause, discontinuation of the offending drug is critical. Switching to an alternative therapy may be considered.
- For infections: Appropriate antiviral or antibiotic treatments are necessary if the pancreatitis is triggered by an infection.
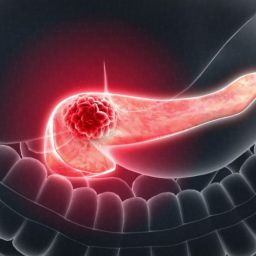
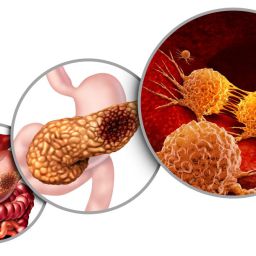
3. Addressing Complications of Acute Pancreatitis
Acute pancreatitis can lead to severe complications, including pancreatic necrosis, organ failure, or infections. Prompt identification and management of these complications are crucial.
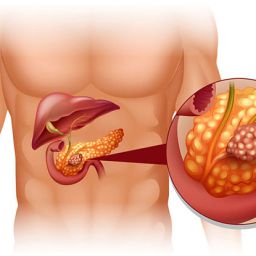
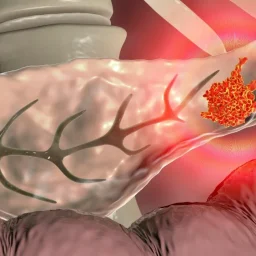
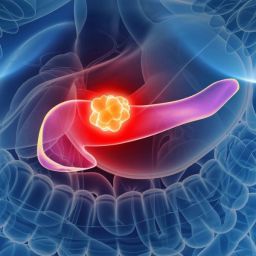
3.1. Pancreatic Necrosis
Pancreatic necrosis occurs when part of the pancreas tissue dies due to severe inflammation. This can lead to infection, which may require surgical intervention. CT scans or MRIs are used to monitor the extent of necrosis, and antibiotics may be prescribed if an infection is suspected.
3.2. Organ Failure
In severe cases, acute pancreatitis can result in multi-organ failure, affecting the lungs, kidneys, heart, and liver. Intensive care may be required for these patients, with measures such as mechanical ventilation, dialysis, and vasopressor support for blood pressure.
3.3. Pseudocysts and Abscesses
Pancreatic pseudocysts (fluid collections around the pancreas) or abscesses (infected fluid collections) can form during recovery. These conditions may require drainage or surgery.
4. Long-Term Management and Lifestyle Modifications
After the acute phase of pancreatitis has passed, it is crucial to prevent future episodes. Long-term management focuses on lifestyle modifications, dietary changes, and follow-up care.
4.1. Dietary Adjustments
- Low-fat diet: After an episode of acute pancreatitis, a low-fat diet is typically recommended to reduce stress on the pancreas. Fats can stimulate the pancreas to secrete digestive enzymes, potentially leading to further irritation.
- Small, frequent meals: Eating smaller meals throughout the day can reduce the strain on the pancreas and improve digestion.
- Avoidance of alcohol: Since alcohol is a significant risk factor for recurrent pancreatitis, it is essential to completely avoid alcoholic beverages.
- High-protein, low-carb foods: Protein-rich foods that are low in fat, such as lean meats, fish, and plant-based proteins, are often recommended. Carbohydrates should be consumed in moderation.
4.2. Smoking Cessation
Smoking is another risk factor that can exacerbate pancreatic diseases. It is crucial for individuals recovering from acute pancreatitis to quit smoking to reduce the risk of recurrence and improve overall health.
4.3. Monitoring for Complications
Ongoing medical follow-up is necessary to monitor for complications, including chronic pancreatitis, diabetes, or pancreatic cancer. Regular blood tests and imaging studies may be required to track the condition and prevent long-term damage.
5. Psychological and Emotional Support
A diagnosis of acute pancreatitis can be physically and emotionally taxing. Many patients may experience anxiety, depression, or fear of future complications. Psychological support, including counseling or therapy, can help patients cope with the emotional stress associated with the condition. Support groups may also provide a sense of community and shared experiences.
6. When Is Surgery Needed?
In some cases, surgery may be required to address complications or underlying causes of acute pancreatitis. These may include:
- Gallbladder removal if gallstones are the cause.
- Drainage procedures for pseudocysts or abscesses.
- Surgical removal of part of the pancreas if extensive damage or pancreatic cancer is suspected.
The diagnosis of acute pancreatitis requires prompt and appropriate medical management to reduce the risk of complications and promote recovery. Following the acute phase, long-term care focuses on lifestyle changes, dietary adjustments, and close monitoring to prevent recurrence and minimize the risk of further damage to the pancreas. With the right treatment plan, individuals can recover from acute pancreatitis and maintain good pancreatic health.
Regular follow-ups, adherence to medical advice, and support from healthcare professionals are critical in ensuring a full recovery and long-term well-being.