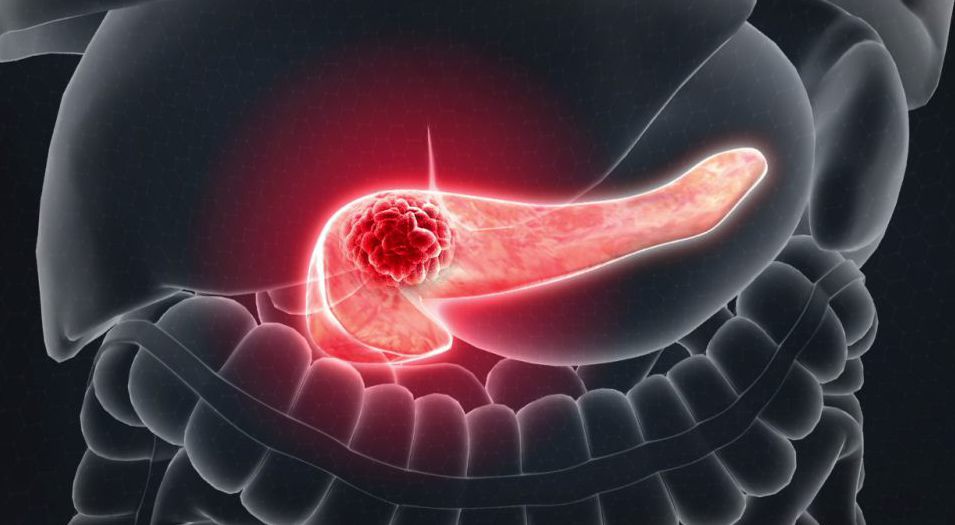
1. Understanding Pancreatic Cancer Progression
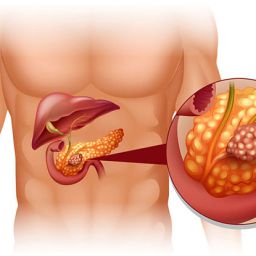
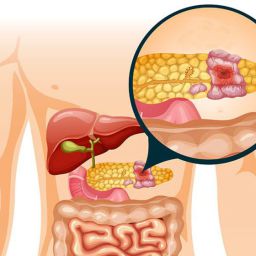
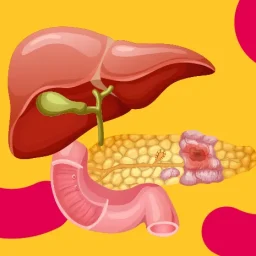
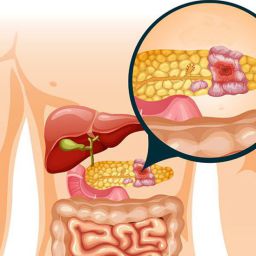
To effectively slow the progression of pancreatic cancer, it is important to understand how the disease develops and spreads. Pancreatic cancer typically begins in the tissues of the pancreas, most commonly in the cells lining the ducts, and can quickly spread to nearby organs, such as the liver, lungs, and lymph nodes.
1.1 Stages of Pancreatic Cancer
- Stage I: The cancer is confined to the pancreas.
- Stage II: The cancer has spread to nearby tissues or lymph nodes.
- Stage III: The cancer has spread to nearby major blood vessels.
- Stage IV: The cancer has spread to distant organs, such as the liver or lungs.
1.2 Factors Affecting Disease Progression
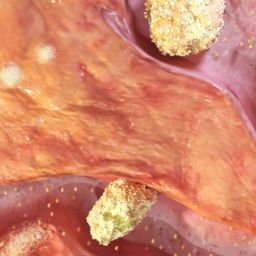
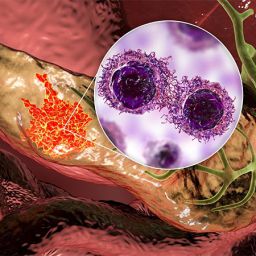
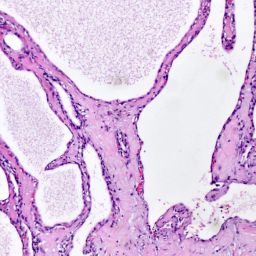
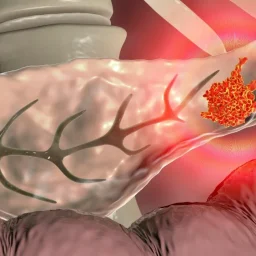
- Genetic Mutations: Mutations in genes such as KRAS, TP53, and CDKN2A play a significant role in pancreatic cancer’s aggressiveness.
- Tumor Microenvironment: The tumor’s microenvironment, including immune cells and blood vessels, can influence how quickly the cancer grows and spreads.
- Patient’s Overall Health: A patient’s age, general health, and immune system function can all impact how the disease progresses.
2. Medical Treatment Options to Slow Disease Progression
The cornerstone of slowing pancreatic cancer progression is through medical treatments that target the cancer cells directly. Various therapies are available depending on the stage of the disease, the patient’s overall health, and the specific characteristics of the cancer.
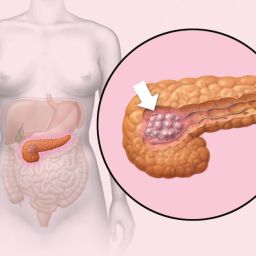
2.1 Surgery: When It’s an Option
- Surgical Resection: The primary goal of surgery is to remove as much of the tumor as possible. In cases where the tumor is confined to the pancreas or localized to nearby structures, surgery may offer the best opportunity to slow or stop cancer progression.
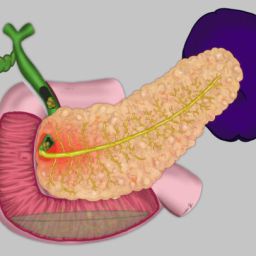
- Whipple Procedure: The most common surgery for pancreatic cancer, also called pancreaticoduodenectomy, involves removing the head of the pancreas, part of the small intestine, the bile duct, and sometimes the stomach.
- Distal Pancreatectomy: In cases where the tumor is located in the tail or body of the pancreas, the distal pancreatectomy may be performed to remove part of the pancreas along with nearby tissue.
- Challenges of Surgery: Surgery may not be possible for patients with advanced cancer due to metastasis. In such cases, surgery can still be used to relieve symptoms such as blockages.
2.2 Chemotherapy
Chemotherapy is the most common treatment used for pancreatic cancer, particularly for patients who are not candidates for surgery. Chemotherapy drugs target rapidly dividing cancer cells, slowing their growth and, in some cases, shrinking the tumor.
- FOLFIRINOX: A combination of drugs that has been shown to improve survival in patients with metastatic pancreatic cancer.
- Gemcitabine: A chemotherapy drug that is often used in combination with other treatments to manage advanced pancreatic cancer.
- Nab-Paclitaxel: Used in combination with gemcitabine, this treatment can slow the growth of the cancer cells.
Chemotherapy is often used to control symptoms, extend survival, and prevent the spread of cancer to other organs.
2.3 Targeted Therapy
Targeted therapy uses drugs that specifically target the genetic mutations and abnormal proteins involved in the growth of cancer cells. These therapies aim to slow the progression of pancreatic cancer by blocking the pathways that allow cancer cells to grow and divide.
- Erlotinib: A targeted drug that inhibits the epidermal growth factor receptor (EGFR), which is involved in the growth and spread of cancer cells.
- PARP Inhibitors: These are used in patients with genetic mutations, such as BRCA1 or BRCA2, to repair DNA damage in cancer cells and prevent them from replicating.
2.4 Immunotherapy
Immunotherapy aims to boost the body’s immune system to better recognize and fight cancer cells. While immunotherapy has shown promise in treating other cancers, its application in pancreatic cancer has been limited. However, ongoing clinical trials are exploring the potential benefits of immunotherapy.
- Checkpoint Inhibitors: Drugs that block immune checkpoints, allowing the immune system to attack the cancer cells more effectively. Keytruda and Opdivo are examples of checkpoint inhibitors.
- Cancer Vaccines: Research is being conducted on vaccines that could help the immune system target pancreatic cancer cells more specifically.
2.5 Radiation Therapy
Radiation therapy uses high-energy beams to kill or shrink cancer cells. It is typically used in combination with surgery or chemotherapy to treat pancreatic cancer. Radiation can help control pain, reduce tumor size, and manage complications related to cancer growth.
- Stereotactic Body Radiation Therapy (SBRT): A more advanced form of radiation therapy that delivers highly focused radiation to tumors while minimizing damage to surrounding healthy tissue.
3. Lifestyle Changes and Complementary Approaches
In addition to medical treatment, certain lifestyle changes can help slow the progression of pancreatic cancer and improve a patient’s overall well-being.
3.1 Diet and Nutrition
Maintaining good nutrition is crucial for pancreatic cancer patients, particularly because the disease and its treatments can cause malnutrition and weight loss. A balanced diet helps to maintain strength, support the immune system, and improve energy levels.

- High-Protein Diets: Pancreatic cancer patients often experience muscle wasting, so it’s important to consume a high-protein diet to preserve lean muscle mass.
- Smaller, More Frequent Meals: Patients may have difficulty eating large meals due to digestive problems, so small, frequent meals can be easier to tolerate.
- Nutritional Supplements: Patients may need additional vitamins, minerals, and enzymes to help with digestion and maintain energy levels.
3.2 Physical Activity
Exercise is important for maintaining physical strength, managing symptoms, and reducing fatigue. Gentle exercises like walking, yoga, or swimming can help improve circulation, reduce pain, and enhance the patient’s mood.
- Rehabilitation Programs: These programs can help improve physical function and mobility after surgery or during chemotherapy.
3.3 Psychological Support
The emotional and psychological toll of a pancreatic cancer diagnosis can be significant. Depression, anxiety, and stress are common among patients. Providing emotional support through counseling, support groups, and stress-relieving activities can help improve quality of life.
- Cognitive Behavioral Therapy (CBT): CBT can help patients manage their thoughts and feelings, reduce anxiety, and improve coping strategies.
- Mindfulness and Meditation: These techniques help patients reduce stress and increase relaxation, improving emotional well-being.
4. Early Detection and Surveillance
Early detection of pancreatic cancer is one of the most important factors in slowing its progression. Unfortunately, pancreatic cancer is often diagnosed in its later stages when it has already spread, making it harder to treat effectively. However, ongoing research and improved diagnostic tools are helping with earlier detection.
4.1 Genetic Testing
For individuals at high risk due to family history or genetic predisposition, genetic testing can help detect mutations that increase the risk of pancreatic cancer, such as BRCA mutations. Early genetic screening and surveillance may allow for earlier detection of the disease.
4.2 Imaging and Biomarkers
Advancements in imaging technologies, such as high-resolution CT scans and MRI, can aid in detecting tumors at an earlier stage. Additionally, research is ongoing into biomarkers that can be used for early detection through blood tests.
While pancreatic cancer remains one of the most difficult cancers to treat, significant advancements in treatment options, lifestyle changes, and early detection methods offer hope for slowing the progression of the disease. Through a combination of medical treatments, nutritional support, physical activity, psychological care, and complementary therapies, it is possible to extend survival and improve the quality of life for pancreatic cancer patients.
By continuing to explore and implement these measures, patients, caregivers, and healthcare providers can work together to manage the disease and slow its progression, offering a better outcome for those affected by pancreatic cancer.