1. Genetic Mutations and Soft Tissue Cancer
Genetic mutations are changes in the DNA sequence that can lead to abnormal cell growth and cancer. These mutations can be either inherited (passed down from one generation to the next) or acquired (developed during a person’s lifetime due to environmental factors or errors during cell division). In soft tissue cancer, both types of mutations can contribute to tumor formation.
A. Inherited Genetic Mutations
Some individuals inherit genetic mutations that increase their susceptibility to developing soft tissue cancers. These inherited mutations are often linked to specific genetic syndromes that predispose individuals to a variety of cancers, including soft tissue sarcomas. For example:

- Li-Fraumeni Syndrome (LFS): Li-Fraumeni syndrome is a rare inherited disorder caused by mutations in the TP53 gene, which encodes the p53 protein, a key regulator of the cell cycle and apoptosis (programmed cell death). Mutations in the TP53 gene lead to a higher risk of developing various cancers, including soft tissue sarcomas, breast cancer, leukemia, and brain tumors. Individuals with Li-Fraumeni syndrome have a significantly increased risk of developing soft tissue sarcomas at an early age, often before the age of 30.
- Neurofibromatosis Type 1 (NF1): Neurofibromatosis type 1 is an inherited condition caused by mutations in the NF1 gene, which encodes a protein called neurofibromin that helps regulate cell growth. People with NF1 are at increased risk of developing a range of benign and malignant tumors, including soft tissue sarcomas such as malignant peripheral nerve sheath tumors (MPNST). MPNSTs often occur in individuals with neurofibromatosis and are known for their aggressive nature and tendency to recur.
- Rothmund-Thomson Syndrome (RTS): Rothmund-Thomson syndrome is a rare genetic disorder associated with mutations in the RECQL4 gene. This syndrome predisposes individuals to a variety of cancers, including soft tissue sarcomas. RTS is characterized by skin abnormalities, bone defects, and a higher risk of developing osteosarcoma and soft tissue sarcomas.
- Gardner’s Syndrome: Gardner’s syndrome is an inherited condition caused by mutations in the APC gene, which is responsible for controlling cell growth. People with Gardner’s syndrome have an increased risk of developing multiple types of cancers, including soft tissue sarcomas, as well as benign growths such as polyps in the colon and skin cysts.
These genetic syndromes, while rare, highlight the important role of inherited genetic mutations in the development of soft tissue cancers. Genetic testing and counseling are essential for individuals with a family history of these syndromes to assess their risk of developing cancer and to implement preventive measures or early detection strategies.
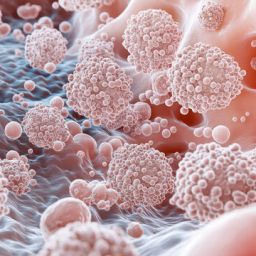
B. Acquired Genetic Mutations
Acquired genetic mutations are changes in the DNA that occur over a person’s lifetime due to factors like exposure to radiation, chemicals, or errors during DNA replication. These mutations are not inherited but develop in the cells during the individual’s life and contribute to the formation of cancer. In soft tissue sarcomas, acquired mutations are the primary cause of most cases, and they typically occur in specific genes involved in regulating the cell cycle, DNA repair, and apoptosis.
One of the most significant genetic alterations found in soft tissue cancers is in the TP53 gene, which is commonly mutated in many different cancer types, including soft tissue sarcomas. When this gene is mutated, it can no longer effectively control the cell cycle or promote the death of damaged cells, allowing the accumulation of additional genetic errors that promote cancer development.
Other common mutations found in soft tissue sarcomas involve genes like MDM2, PDGFRA, KIT, and FGFR1, which play roles in cell growth, survival, and differentiation. These mutations can lead to the uncontrolled growth of cells, resulting in the formation of a sarcoma.
2. Genetic Syndromes Associated with Soft Tissue Cancer
In addition to the inherited mutations mentioned above, certain genetic syndromes are closely associated with the development of soft tissue cancer. These syndromes can predispose individuals to multiple types of cancer, including soft tissue sarcomas.
A. Li-Fraumeni Syndrome (LFS)
As mentioned earlier, Li-Fraumeni syndrome is an inherited disorder caused by mutations in the TP53 gene. Individuals with LFS are at a higher risk of developing soft tissue sarcomas, such as rhabdomyosarcoma, as well as other cancers like breast cancer, brain tumors, and leukemia. The presence of a TP53 mutation makes individuals more susceptible to cancer at a young age, often in childhood or adolescence.
B. Neurofibromatosis Type 1 (NF1)
NF1 is a genetic disorder caused by mutations in the NF1 gene. This syndrome is associated with an increased risk of developing soft tissue sarcomas, particularly malignant peripheral nerve sheath tumors (MPNSTs). These tumors arise from the peripheral nerves and are commonly seen in individuals with neurofibromatosis. MPNSTs are aggressive and often have a poor prognosis, especially if not detected early.
C. Werner Syndrome
Werner syndrome, caused by mutations in the WRN gene, is another genetic condition that predisposes individuals to soft tissue sarcomas. This syndrome leads to premature aging and increases the risk of several types of cancer, including sarcomas. It is rare, but individuals with Werner syndrome may develop soft tissue tumors, particularly in the second or third decade of life.
D. Retinoblastoma (RB) Gene Mutations
Retinoblastoma is a childhood cancer that typically affects the retina of the eye. Mutations in the RB1 gene can also predispose individuals to other cancers, including soft tissue sarcomas. People with inherited mutations in the RB1 gene may develop a variety of cancers, including osteosarcoma, rhabdomyosarcoma, and soft tissue tumors.
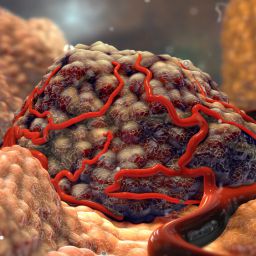
3. Molecular Mechanisms in Soft Tissue Cancer
The development of soft tissue cancers is driven by a complex interplay of genetic mutations and molecular pathways that regulate normal cell function. In soft tissue sarcomas, these molecular changes often involve the disruption of signaling pathways that control cell growth, differentiation, survival, and apoptosis.
A. Tumor Suppressor Genes
Tumor suppressor genes, such as TP53, RB1, and NF1, play essential roles in regulating the cell cycle and preventing uncontrolled cell division. Mutations in these genes are common in soft tissue cancers and can lead to the development of sarcomas by allowing cells to evade normal growth controls.
B. Oncogenes
Oncogenes are genes that promote cell division and survival. When these genes are mutated or overexpressed, they can drive tumorigenesis. In soft tissue cancers, oncogenes like MDM2, PDGFRA, and KIT are frequently altered, leading to excessive cell proliferation and resistance to cell death.
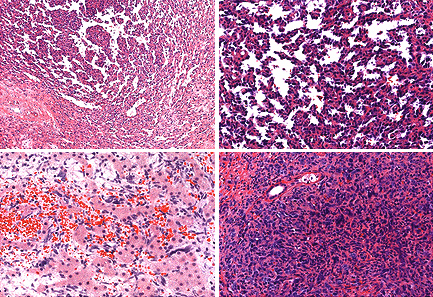
C. Chromosomal Rearrangements
Many soft tissue sarcomas are characterized by specific chromosomal rearrangements that result in the fusion of two genes. For example, synovial sarcoma is often associated with a translocation between chromosomes X and 18, leading to the formation of the SYT-SSX fusion gene. These genetic rearrangements drive the growth of tumors and are important for diagnosing specific subtypes of soft tissue sarcomas.
4. Genetic Testing and Its Role in Diagnosis
Genetic testing plays a critical role in the diagnosis and management of soft tissue cancers. With advances in genomic technologies, including next-generation sequencing (NGS), it is now possible to identify specific genetic mutations and alterations in soft tissue sarcomas that can guide treatment decisions.
A. Identifying Genetic Mutations
Genetic tests can help identify mutations in key tumor suppressor genes, oncogenes, and chromosomal rearrangements associated with soft tissue sarcomas. This information can provide insights into the type of sarcoma, its likely behavior, and the best treatment approach.
B. Personalized Medicine
As the field of personalized medicine continues to evolve, genetic testing can help identify targeted therapies based on the genetic profile of the tumor. For example, some soft tissue sarcomas with mutations in the KIT gene may respond to targeted therapies that inhibit the activity of the KIT protein. Similarly, drugs that target specific genetic mutations or pathways involved in the development of sarcomas are being developed and tested in clinical trials.
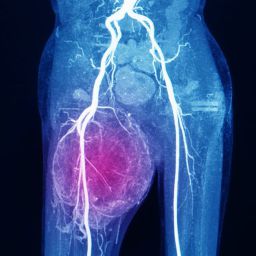
5. Implications for Treatment and Prognosis
Understanding the genetic basis of soft tissue cancers has significant implications for treatment and prognosis. Targeted therapies, immunotherapies, and precision medicine approaches are increasingly being used to treat soft tissue sarcomas, offering hope for improved outcomes and fewer side effects compared to traditional chemotherapy and radiation.
In addition, genetic counseling is essential for patients and their families to understand their risk of developing soft tissue cancer and the potential for passing on inherited mutations to future generations.
Genetic factors play a critical role in the development of soft tissue cancers, influencing both the risk of tumor formation and the behavior of the cancer. Inherited mutations, genetic syndromes, and acquired mutations all contribute to the development of soft tissue sarcomas, making genetic testing and counseling essential in managing these cancers. By understanding the genetic underpinnings of these cancers, we can move toward more personalized and effective treatment options, improving the prognosis for patients with soft tissue sarcomas.
Advancements in genomics, molecular biology, and targeted therapies continue to offer hope for patients with soft tissue cancer. As research progresses, the role of genetic factors will likely become even more prominent in shaping the future of cancer diagnosis, treatment, and prevention.