
1. Understanding PIPAC Treatment
PIPAC is a relatively novel approach in the administration of chemotherapy. Unlike traditional chemotherapy, which is delivered intravenously or directly into the affected area, PIPAC uses a unique aerosol delivery system. It administers chemotherapy drugs directly to the peritoneal cavity via a pressurized aerosol spray. This method maximizes the drug’s penetration into the tumor tissues within the peritoneum while minimizing systemic toxicity, leading to potentially fewer side effects compared to conventional chemotherapy.
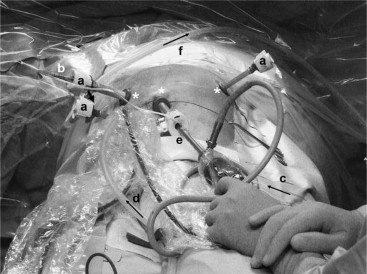
The process involves the introduction of chemotherapy agents as a fine aerosol mist into the peritoneal cavity under pressure during a laparoscopic procedure. The pressurized environment allows for deeper penetration of the chemotherapy drugs into the peritoneal tumors, increasing the efficacy of the treatment while preserving healthy surrounding tissue.
2. Clinical Applications of PIPAC

The primary clinical application of PIPAC is in the treatment of peritoneal carcinomatosis (PC), a condition where cancer cells spread to the lining of the abdominal cavity (the peritoneum). PC can be caused by various cancers, including colorectal, gastric, ovarian, pancreatic, and endometrial cancers. These cancers often metastasize to the peritoneum and are difficult to treat with traditional chemotherapy or surgery.
Traditional systemic chemotherapy may not be as effective for treating cancers confined to the peritoneum due to its limited ability to reach the peritoneal surface. PIPAC overcomes this limitation by delivering chemotherapy directly to the site of the cancer, improving local drug concentration and potentially reducing the need for systemic chemotherapy.
In addition to peritoneal carcinomatosis, PIPAC is also being explored in the treatment of other abdominal cancers, such as those originating from the ovaries, stomach, and pancreas. Ongoing clinical trials are testing its effectiveness in various cancer types, including colorectal and breast cancers with peritoneal spread.
3. Benefits of PIPAC
There are several benefits to PIPAC, making it an attractive option in cancer therapy, particularly in cases where conventional treatments have proven less effective.
a. Targeted Treatment: One of the most significant advantages of PIPAC is its ability to directly target tumors in the peritoneum. The aerosolized chemotherapy reaches areas of the abdominal cavity that might be missed by traditional methods, allowing for more precise treatment.
b. Minimizing Systemic Toxicity: Since PIPAC delivers chemotherapy directly to the affected area, it significantly reduces the risk of systemic side effects. Traditional chemotherapy affects the entire body, leading to side effects such as nausea, hair loss, and fatigue. With PIPAC, chemotherapy is confined to the peritoneal cavity, decreasing the burden on other organs and minimizing adverse effects.
c. Laparoscopic Approach: PIPAC is performed through a minimally invasive laparoscopic procedure, meaning that patients experience smaller incisions, less postoperative pain, and faster recovery times. Laparoscopy also allows for real-time visualization of the peritoneal cavity and precise administration of the treatment.
d. Potential for Repeated Treatments: In patients with peritoneal carcinomatosis, chemotherapy may need to be repeated multiple times to control tumor growth. PIPAC’s aerosolized approach makes it possible to administer the treatment multiple times, improving its long-term effectiveness without significant harm to the surrounding healthy tissues.
e. Efficacy in Advanced Cases: PIPAC has shown promise in patients with advanced-stage cancers that are not candidates for curative surgery. It provides an additional option for managing cancer progression, potentially prolonging survival and improving the quality of life for patients with otherwise limited treatment options.
4. PIPAC vs. Traditional Chemotherapy and Other Treatments
Traditional chemotherapy for peritoneal carcinomatosis is often administered systemically, with limited success in delivering the required dose of chemotherapy to the peritoneal tumors. Chemotherapy agents delivered intravenously are diluted as they circulate through the bloodstream, making it challenging to achieve effective concentrations in the peritoneal cavity. Moreover, systemic chemotherapy comes with a high incidence of severe side effects due to the toxic effects on healthy tissues.
In contrast, PIPAC directly targets the peritoneal tumors, allowing for higher local concentrations of chemotherapy drugs and sparing healthy tissues from exposure to toxic doses. It also offers the benefit of a laparoscopic approach, which is less invasive compared to open surgical procedures. The pressurized aerosol system ensures deeper drug penetration, a critical factor for patients with peritoneal spread.
When compared to Hyperthermic Intraperitoneal Chemotherapy (HIPEC), another treatment for peritoneal cancers, PIPAC is generally considered less invasive and may be suitable for patients who cannot undergo the more extensive HIPEC procedure. HIPEC requires open surgery, and its use is typically limited to patients who are in better overall health and whose cancer has been surgically resected.
5. Side Effects and Challenges of PIPAC Treatment
Despite its potential benefits, PIPAC treatment is not without challenges and risks. While the targeted delivery of chemotherapy reduces systemic side effects, patients may still experience some local side effects in the abdominal area. These may include:
- Abdominal pain or discomfort
- Nausea or vomiting
- Fever
- Temporary swelling or fluid buildup in the abdomen
- Risk of infection at the incision sites
These side effects are typically short-term and resolve over time. However, in rare cases, more severe complications, such as perforation of the bowel, can occur during the laparoscopic procedure.
Another challenge is the limited long-term data on the efficacy of PIPAC. While early clinical studies have shown promising results, more research is needed to fully assess its long-term impact on survival rates, quality of life, and overall effectiveness in various cancer types. As such, PIPAC is still considered an experimental treatment and is primarily available within clinical trials.
6. The Future of PIPAC in Cancer Treatment
The future of PIPAC in cancer therapy looks promising, with ongoing clinical trials examining its potential in various cancer types. Researchers are exploring combinations of PIPAC with other treatments such as immunotherapy, targeted therapy, and radiation therapy to improve its effectiveness further.
One area of future research involves refining the aerosol delivery system to enhance drug penetration and improve the targeting of specific cancer cells. Additionally, studies are investigating how PIPAC may be integrated into multimodal treatment strategies, where it can be used in conjunction with surgery, radiation therapy, and systemic chemotherapy.
Furthermore, expanding the range of cancers treated with PIPAC could open up new avenues for patients with advanced-stage disease. For instance, combining PIPAC with novel molecular-targeted therapies could offer a powerful approach to fighting cancers that were previously considered difficult or impossible to treat.
PIPAC represents a significant advancement in the treatment of peritoneal carcinomatosis and other abdominal cancers. By delivering chemotherapy directly to the affected areas through a minimally invasive procedure, PIPAC provides a targeted treatment option with potentially fewer side effects compared to traditional chemotherapy. Its benefits in terms of local drug delivery, reduced systemic toxicity, and enhanced drug penetration make it an attractive option for patients with advanced abdominal cancers, particularly those who may not be candidates for traditional treatments or surgery.
While more research is required to establish its long-term efficacy and optimal use, PIPAC’s role in cancer treatment continues to evolve. As clinical trials and studies progress, PIPAC may become a standard part of the oncologist’s toolkit for managing peritoneal cancers, offering hope to patients with limited options for traditional treatments.

