Desmoid tumors are characterized by an abnormal growth of fibrous tissue, resulting in a firm, often painless mass. Though these tumors are classified as benign, they can behave aggressively by infiltrating surrounding tissues, including muscles, nerves, and organs. The exact cause of desmoid tumors is not entirely understood, but they are believed to result from genetic mutations that affect the regulation of cell growth.
In some cases, desmoid tumors are associated with genetic conditions, such as familial adenomatous polyposis (FAP), a hereditary disorder that predisposes individuals to various types of tumors, including desmoid tumors. In these patients, the risk of developing desmoid tumors increases significantly, and these tumors tend to be more aggressive in nature.
Desmoid tumors can occur at any age but are most commonly diagnosed in individuals between the ages of 15 and 60. Women are more frequently affected than men, and pregnancy or hormonal changes can sometimes trigger the development or growth of desmoid tumors, particularly in those who are genetically predisposed.
1. Surgical Intervention for Desmoid Tumors
Surgical excision is the primary treatment option for desmoid tumors, particularly when the tumor is causing symptoms, such as pain or functional impairment, or when the tumor’s size poses a risk to surrounding organs or tissues. The main goal of surgery is to remove the tumor entirely, including any surrounding tissue that may be infiltrated by the tumor cells.
1.1 Surgical Approaches
There are several surgical approaches used for desmoid tumors, depending on the tumor’s location, size, and relationship to surrounding structures:
- Wide Local Excision (WLE): This is the standard surgical technique for desmoid tumors. In wide local excision, the tumor is removed along with a margin of healthy tissue around it to ensure that no cancerous cells are left behind. This approach is typically used for tumors located in easily accessible areas, such as the limbs or subcutaneous tissues.
- Radical Surgery: In cases where desmoid tumors are deeply located or have grown into vital organs or structures, more extensive surgery may be required. This can involve the removal of adjacent tissues, muscles, or organs to ensure that the tumor is fully excised.
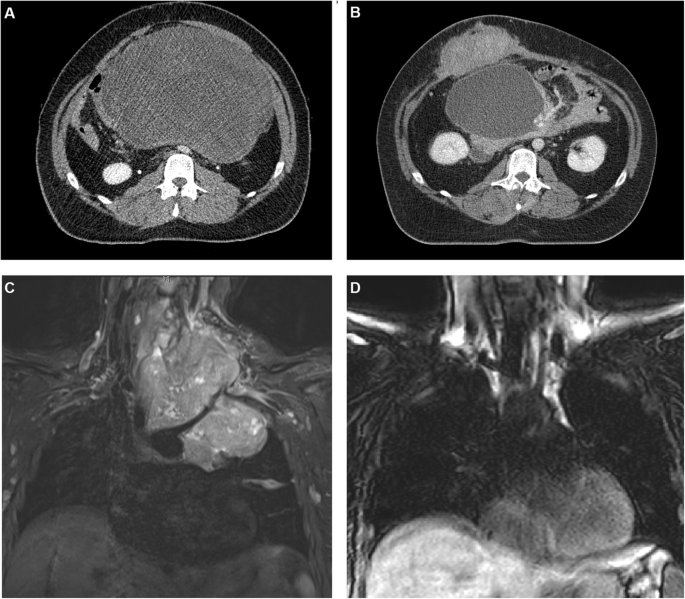
- Minimally Invasive Surgery: In some cases, minimally invasive techniques, such as laparoscopic or robotic surgery, may be used, particularly for abdominal desmoid tumors. These techniques offer smaller incisions and a faster recovery time but may not be suitable for all patients or tumor locations.
Despite the benefits of surgical intervention, the risk of recurrence after surgery remains a significant concern, as desmoid tumors have a well-established tendency to return even after seemingly complete excision.
2. Risk Factors for Recurrence After Surgery
The recurrence of desmoid tumors following surgery is common, and several factors influence the likelihood of recurrence. These include tumor-related factors, patient characteristics, and surgical factors. Understanding these risk factors is crucial for predicting outcomes and developing strategies to prevent recurrence.
2.1 Tumor Characteristics
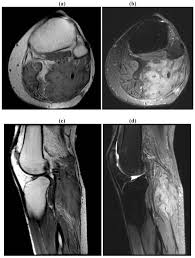
- Tumor Size: Larger desmoid tumors, particularly those greater than 5 cm in diameter, are more likely to recur after surgical excision. Larger tumors are also more likely to invade surrounding tissues, making complete excision more challenging.
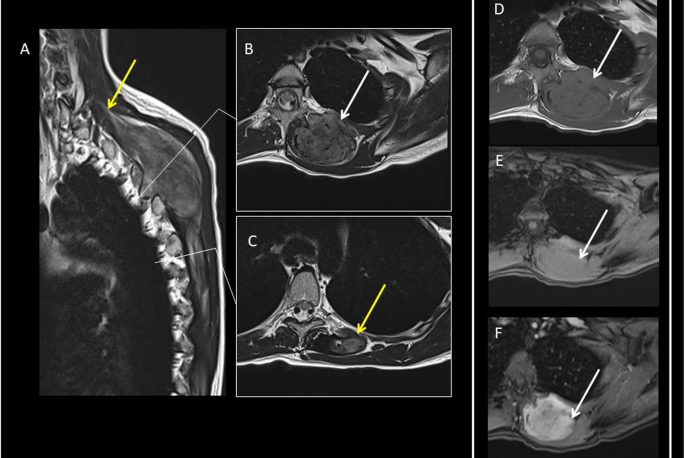
- Tumor Location: The location of the tumor plays a crucial role in the risk of recurrence. Desmoid tumors located in areas with complex anatomical structures, such as the abdominal cavity, pelvis, or retroperitoneum, are more challenging to remove completely. In these locations, tumors are often in close proximity to vital organs, blood vessels, and nerves, making it difficult to ensure clear margins during surgery.
- Tumor Histology: Certain histological features of desmoid tumors are associated with a higher risk of recurrence. Tumors that are more cellular, with less collagen production, tend to be more aggressive and have a higher recurrence rate. Tumors that exhibit infiltrative growth patterns are also more difficult to remove completely, increasing the likelihood of recurrence.
2.2 Surgical Factors
- Incomplete Resection: One of the most important factors contributing to recurrence is the incomplete resection of the tumor. If the surgical margins are not clear, or if tumor cells are left behind, the likelihood of recurrence increases. In some cases, even when the tumor appears to be fully excised, microscopic residual tumor cells can remain and cause regrowth.
- Difficulty Achieving Negative Margins: In cases where desmoid tumors are deeply located or have grown into adjacent organs, it can be challenging to achieve negative surgical margins. Even small amounts of residual tumor tissue can lead to recurrence. Surgeons may need to make difficult decisions about whether to remove surrounding tissues or organs to achieve clear margins, which can affect the patient’s long-term health.
- Post-Surgical Wound Complications: In some cases, complications such as wound infection or delayed wound healing can increase the risk of recurrence. Any surgical complication that results in tissue necrosis or poor healing may compromise the effectiveness of the surgery and increase the likelihood of tumor regrowth.
2.3 Genetic and Hormonal Factors
Patients with familial adenomatous polyposis (FAP) syndrome or those with a family history of desmoid tumors are at a higher risk of recurrence. In these cases, the genetic mutations associated with desmoid tumor formation may also contribute to the tumor’s recurrence, as the underlying genetic predisposition remains present.
Hormonal factors, particularly estrogen, have been shown to influence the growth and recurrence of desmoid tumors. Pregnant women and individuals undergoing hormone therapy may experience tumor growth or recurrence, as the hormonal fluctuations can stimulate the growth of desmoid tissue.
3. Prevention of Recurrence: Strategies and Approaches
While recurrence of desmoid tumors is common, several strategies can be employed to minimize the risk of recurrence and improve long-term outcomes. These strategies include careful surgical planning, adjuvant therapies, and close post-surgical monitoring.

3.1 Surgical Considerations
- Achieving Negative Margins: The most important factor in preventing recurrence is ensuring negative surgical margins. Surgeons should aim for wide excision of the tumor with a margin of healthy tissue to ensure that no tumor cells are left behind. In cases where negative margins are difficult to achieve, multidisciplinary teams of surgeons, oncologists, and radiologists should collaborate to determine the most appropriate course of action.
- Reconstruction and Rehabilitation: After the tumor has been surgically excised, reconstructive surgery may be necessary to restore the function of affected areas. This is particularly true for desmoid tumors that involve the muscles or organs. Rehabilitation, including physical therapy, can help improve recovery and reduce the risk of complications that might contribute to recurrence.
3.2 Adjuvant Therapies
- Radiation Therapy: In some cases, radiation therapy is used after surgery to reduce the risk of recurrence, particularly in patients with positive surgical margins or tumors that are difficult to resect completely. Radiation can help destroy any residual tumor cells that may have been left behind during surgery. However, the use of radiation therapy is typically reserved for cases where surgery alone is not sufficient to prevent recurrence.
- Pharmacological Approaches: Medications that target the tumor’s molecular pathways are being explored as potential treatments for desmoid tumors. Drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs), chemotherapy agents, and newer molecular-targeted therapies may help reduce the risk of recurrence by inhibiting tumor growth and proliferation.
- Hormonal Therapy: Given the influence of estrogen on desmoid tumors, hormonal therapy may be considered in some cases, especially for patients with tumors that are hormonally sensitive. Drugs that block estrogen or reduce hormone levels may help prevent tumor recurrence in certain patients.
3.3 Monitoring and Follow-Up
Regular monitoring and follow-up care are critical in detecting recurrence at an early stage. Patients who have undergone surgery for desmoid tumors should be closely monitored with periodic imaging studies, such as MRI or CT scans, to detect any signs of tumor regrowth. Blood tests may also be used to monitor for markers that indicate the presence of recurrence.
Desmoid tumors pose a unique challenge for both patients and healthcare providers due to their tendency to recur after surgical excision. While surgery is the primary treatment for desmoid tumors, the risk of recurrence remains high, especially for large, deeply located tumors or those with difficult-to-achieve negative margins. The key to preventing recurrence lies in careful surgical planning, achieving clear margins, and employing adjuvant therapies when necessary.
Close follow-up care and monitoring are essential for detecting recurrence at an early stage, allowing for prompt intervention and treatment. While the recurrence of desmoid tumors can be distressing, advancements in surgical techniques, pharmacological treatments, and radiation therapy offer hope for improved outcomes and better long-term management of the disease.
