Etiology and Life Cycle of Echinococcus
Echinococcosis is caused by tapeworms of the genus Echinococcus, with the two most common species being Echinococcus granulosus and Echinococcus multilocularis. These parasites have a complex life cycle that involves both definitive and intermediate hosts. The definitive hosts are typically carnivores such as dogs, wolves, and foxes, while the intermediate hosts are herbivores, including sheep, cattle, and humans.
- Definitive Hosts: Adult tapeworms reside in the intestines of carnivores. The tapeworms release their eggs through feces, which contaminate the environment and water sources.
- Intermediate Hosts: Herbivores (including humans) ingest the eggs through contaminated food, water, or contact with infected animals. Once ingested, the eggs hatch and release larvae that penetrate the intestinal wall and migrate to various organs, primarily the liver and lungs, where they develop into cysts.
- Human Infections: Humans are accidental intermediate hosts who become infected when they ingest the eggs, usually from contaminated water or food or through contact with infected animals.
The larvae grow into large fluid-filled cysts, which can expand over time. These cysts can cause significant damage to the affected organ if left untreated, particularly in the liver, which is the most common site of infection.
Epidemiology of Liver Echinococcosis
Liver echinococcosis is prevalent in areas with close contact between humans, livestock, and dogs, particularly in rural regions. The disease is most common in countries of the Mediterranean region, Central Asia, South America, the Middle East, and parts of Africa. In these regions, human-to-animal transmission cycles are more frequent due to the agricultural lifestyle and the presence of stray dogs.
The incidence of the disease is largely influenced by environmental, socioeconomic, and cultural factors. Poor hygiene practices, the consumption of unwashed vegetables or water, and the proximity of livestock to humans contribute to the spread of Echinococcus eggs. In many cases, the disease remains asymptomatic for years, allowing it to progress unnoticed until it causes significant damage to the liver or other organs.
Symptoms of Liver Echinococcosis
The clinical presentation of liver echinococcosis can vary depending on the size and location of the cysts, as well as the stage of infection. In the early stages, many individuals experience no symptoms, as the cysts develop slowly. However, as the cysts grow and cause pressure on surrounding structures, they may lead to the following symptoms:
- Abdominal Pain: Often localized to the right upper quadrant, abdominal pain occurs when the cysts press against the liver or other nearby organs. The pain can be dull or sharp and may become more pronounced after eating.
- Jaundice: As cysts expand within the liver, they can obstruct bile ducts, leading to the buildup of bile in the bloodstream and causing jaundice (yellowing of the skin and eyes).
- Nausea and Vomiting: These symptoms are common due to the discomfort caused by the enlarging cysts or the effect on liver function.
- Fever and Sweats: In some cases, individuals may experience fever, especially if secondary infections or complications such as cyst rupture occur.
- Fatigue and Weakness: As the disease progresses, patients may feel generally weak or fatigued due to liver dysfunction.
- Palpable Mass: In some cases, the liver may become enlarged, and a palpable mass can be felt during physical examination, particularly in individuals with larger cysts.
Complications of Liver Echinococcosis
If left untreated, liver echinococcosis can lead to several severe complications:
- Cyst Rupture: The cysts may rupture, leading to the spread of Echinococcus larvae into the abdominal cavity. This can cause anaphylactic shock and result in a potentially life-threatening condition. In some cases, the rupture can cause an infection or lead to the formation of new cysts in other parts of the body.
- Liver Dysfunction: Large cysts can interfere with liver function, causing hepatic insufficiency, which may require a liver transplant if the damage is extensive.
- Biliary Obstruction: The cysts can obstruct the bile ducts, leading to biliary cirrhosis or cholangitis, which further complicates the condition.
- Metastasis to Other Organs: Although rare, in severe cases, the larvae can spread from the liver to other organs such as the lungs, brain, or kidneys, where new cysts can form, complicating treatment.
Diagnostic Methods for Liver Echinococcosis
The diagnosis of liver echinococcosis can be challenging due to the asymptomatic nature of the disease in its early stages. A combination of clinical suspicion, imaging techniques, and serological tests is typically used to confirm the diagnosis.
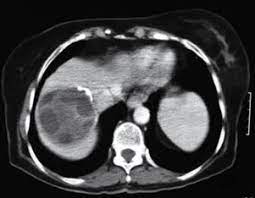
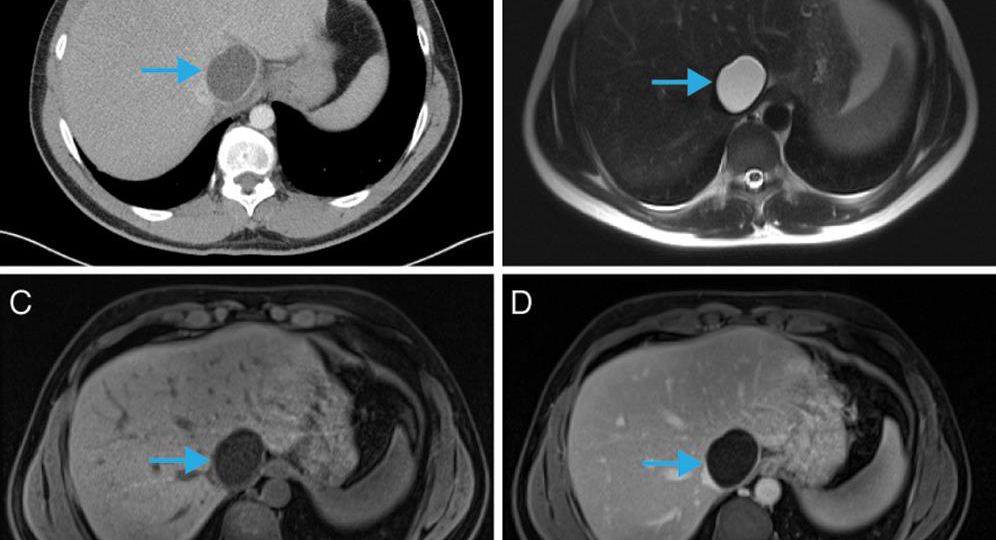
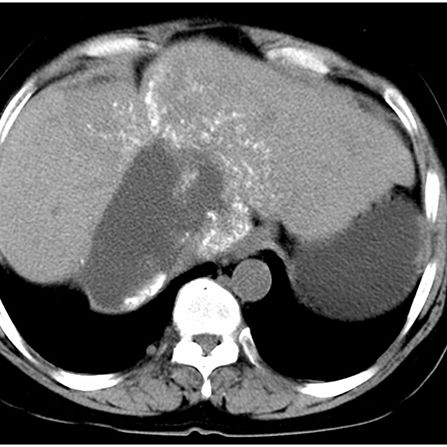
- Ultrasound Imaging: The primary diagnostic tool for identifying liver cysts. Ultrasound can reveal the presence, size, and location of the cysts and help distinguish them from other liver lesions.
- CT Scan (Computed Tomography): Provides more detailed images of the liver and surrounding organs, helping to assess the size, number, and potential complications of the cysts. CT scans are often used to guide biopsy or surgical planning.
- MRI (Magnetic Resonance Imaging): MRI is useful in providing detailed images, especially when differentiating between echinococcal cysts and other liver conditions.
- Serological Tests: Blood tests can detect the presence of antibodies specific to Echinococcus. Elevated levels of specific IgG antibodies may indicate active infection, although false positives can occur.
- Histopathological Examination: A biopsy of the cyst, obtained via needle aspiration or during surgery, can help confirm the diagnosis by identifying the presence of Echinococcus larvae.
Treatment of Liver Echinococcosis
The treatment of liver echinococcosis depends on several factors, including the size, location, and number of cysts, as well as the patient’s overall health. The main treatment options include:
- Surgical Intervention: Surgical removal of the cysts is the most effective treatment for liver echinococcosis. This can be done through traditional open surgery or minimally invasive techniques, such as laparoscopic surgery. In some cases, liver transplantation may be required if extensive liver damage has occurred.
- Percutaneous Aspiration and Injection (PAIR): A minimally invasive procedure in which the cyst is aspirated, and then a sclerosing agent (such as ethanol or hypertonic saline) is injected into the cyst to kill the larvae. This method is suitable for certain cysts that are difficult to reach surgically.
- Anthelmintic Medications: Drugs such as albendazole and mebendazole can be used to kill the larvae and prevent the growth of new cysts. These medications are typically used in combination with surgery or when surgery is not an option.
- Supportive Care: In cases where surgery is not possible or complications arise, supportive care is provided to manage symptoms and maintain liver function.
Prevention of Liver Echinococcosis
Preventing liver echinococcosis involves reducing the risk of exposure to Echinococcus eggs. Key preventive measures include:
- Proper Hygiene and Sanitation: Washing hands thoroughly after handling animals, especially dogs, and ensuring proper sanitation in areas where livestock is raised.
- Controlling Stray Dogs: Stray dogs should be managed and prevented from roaming near livestock or human settlements.
- De-worming of Dogs: Regular de-worming of domestic dogs and livestock is an essential preventive measure.
- Food and Water Safety: Ensuring that vegetables, fruits, and drinking water are thoroughly washed and free from contamination.
- Public Awareness: Educating rural populations, particularly those in endemic areas, about the risks of echinococcosis and the necessary precautions to prevent infection.
Liver echinococcosis remains a significant health concern, particularly in regions where close contact between humans, livestock, and dogs is common. Early diagnosis, appropriate treatment, and effective preventive measures can reduce the morbidity and mortality associated with this parasitic infection. Understanding its pathophysiology, symptoms, diagnostic methods, and treatment options is crucial for managing and preventing liver echinococcosis, ultimately improving patient outcomes and quality of life.