1. Understanding Bloating After Appendectomy
Bloating refers to a sensation of fullness or swelling in the abdomen, often accompanied by discomfort, gas, and sometimes visible distention. After an appendectomy, bloating is a common symptom that many patients experience to varying degrees. The bloating can range from mild to severe and can persist for several days to weeks after surgery.
Causes of Bloating After Appendectomy:

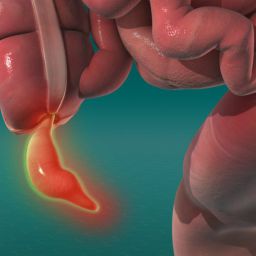
- Surgical Manipulation of the Abdomen: During an appendectomy, the surgeon makes incisions in the abdominal area to remove the appendix. Even in minimally invasive (laparoscopic) surgery, gas is often introduced into the abdomen to create space for the surgeon to work. This gas (usually carbon dioxide) may take time to be absorbed or expelled from the body, leading to a sensation of bloating or discomfort. The surgical manipulation of tissues and organs can also lead to temporary disruption in the normal function of the digestive system.
- Anesthesia and Medications: Anesthesia used during surgery, as well as post-operative pain medications (like opioids), can slow down the digestive system. This delay in bowel movement and gastric motility can lead to a buildup of gas, causing bloating. Narcotic pain medications, in particular, are known to cause constipation and abdominal discomfort, which can contribute to the sensation of fullness and swelling.
- Reduced Physical Activity: After surgery, patients are advised to rest and avoid physical exertion to ensure proper healing. This lack of movement can lead to slower digestion and decreased gastrointestinal motility, which contributes to bloating. Normal physical activity, such as walking, helps promote digestion and the expulsion of gas from the intestines.
- Dietary Changes: Post-surgery, patients may be instructed to follow a specific diet as their digestive system adjusts. This may include a gradual reintroduction of foods, often starting with liquids and moving to soft foods. However, changes in diet, such as consuming new or softer foods that are easier to digest, can sometimes lead to temporary gas buildup and bloating as the stomach and intestines adjust.
2. How Bloating Affects Post-Appendectomy Recovery
While bloating is typically a temporary issue, it can affect a patient’s recovery and overall comfort after an appendectomy. Some of the ways bloating impacts recovery include:
Discomfort and Pain:
Abdominal bloating can cause mild to moderate pain and discomfort in the abdominal area. This pain may be exacerbated by movement, breathing deeply, or coughing, which are necessary for post-surgical recovery. This discomfort can sometimes overlap with the normal healing pain from the surgical site, making it more difficult for patients to distinguish between the two sources of pain.
Reduced Appetite:
Bloating can make patients feel full, even if they haven’t eaten much. This sensation can reduce appetite, making it more difficult for patients to maintain proper nutrition during the recovery process. Since adequate nutrition is critical for healing and immune function, a decreased appetite can potentially delay recovery if not managed properly.
Increased Stress and Anxiety:
Bloating, especially if it leads to visible distention of the abdomen, can cause anxiety or stress. Patients recovering from surgery are already under physical and emotional strain, and the added discomfort of bloating can exacerbate these feelings, making recovery more difficult.
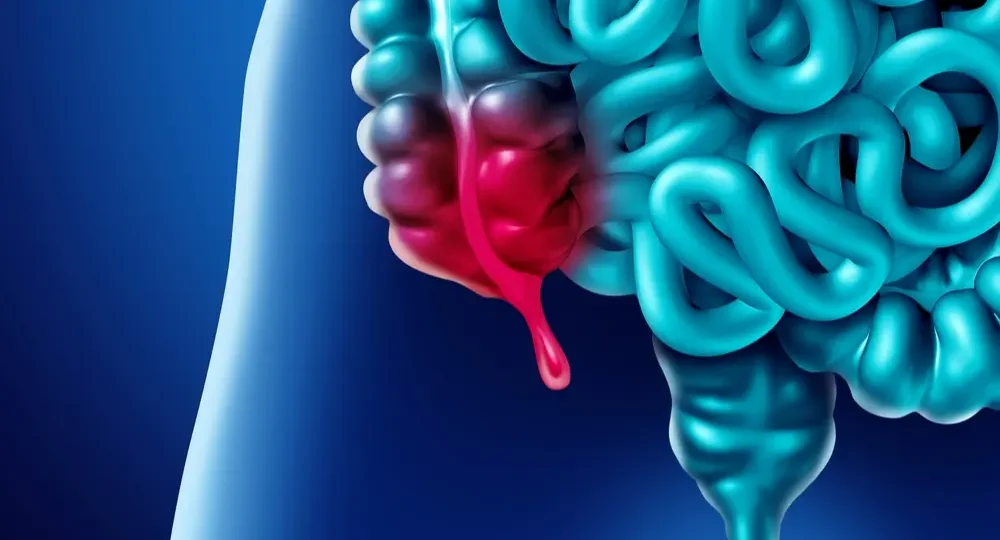
Delayed Digestive Function:
In some cases, bloating can be a sign of delayed gastric emptying or constipation. If left unaddressed, this can lead to more severe digestive issues, such as prolonged constipation, nausea, or vomiting, which may require additional medical intervention.
3. Preventing and Managing Bloating After Appendectomy
While bloating after appendectomy is often inevitable, there are several strategies patients can use to prevent or minimize its occurrence. These strategies focus on reducing the impact of the underlying causes of bloating and promoting digestive health during recovery.

Post-Operative Care and Mobility:
- Early Mobilization: One of the most effective ways to reduce bloating after appendectomy is to begin moving around as soon as it is safe to do so. Walking, even short distances, can promote the movement of gas through the intestines and help stimulate bowel function. Early mobilization not only improves digestion but also reduces the risk of complications such as blood clots and pneumonia.
- Gentle Exercises: Once permitted by the surgeon, light exercises like stretching and walking can help improve overall circulation and digestive motility. This promotes the movement of gas through the digestive system and prevents the buildup of bloating.
Dietary Modifications:
- Gradual Reintroduction of Foods: After surgery, patients are typically advised to follow a specific diet that begins with clear liquids and gradually progresses to soft foods. It is essential to avoid introducing solid foods too quickly, as this can overwhelm the digestive system and contribute to bloating.
- Avoiding Gas-Producing Foods: Certain foods are known to cause excess gas and bloating, including beans, carbonated beverages, cruciferous vegetables (like broccoli, cabbage, and cauliflower), and fatty foods. During the first few weeks after surgery, patients should limit or avoid these foods to reduce the risk of bloating.
- Small, Frequent Meals: Eating smaller meals more frequently can help reduce the sensation of fullness and bloating. Larger meals may take longer to digest, leading to more discomfort. By eating smaller portions, the digestive system is better able to manage food intake and prevent the buildup of gas.
- Hydration: Drinking plenty of fluids, especially water, can aid in digestion and prevent constipation, which is a major contributor to bloating. Hydration also helps the body flush out any remaining gas in the digestive tract.
Managing Medications:
- Pain Medication Adjustments: Opioid-based pain medications are commonly prescribed after appendectomy, but they can slow down digestion and lead to bloating. Patients should discuss alternative pain management options with their healthcare provider. Non-narcotic pain relief methods, such as acetaminophen, may be less likely to cause constipation and digestive issues.
- Laxatives or Stool Softeners: If constipation becomes an issue, stool softeners or mild laxatives may be recommended to facilitate bowel movements. However, these should only be used under the guidance of a healthcare provider to avoid overuse or dependency.
Breathing Exercises:
Deep breathing exercises are a helpful technique for reducing abdominal discomfort and bloating. Slow, deep breaths help relax the abdominal muscles and can reduce the sensation of fullness. Additionally, controlled breathing may help release trapped gas in the intestines, which contributes to bloating.
4. When to Seek Medical Attention
While bloating is typically a minor issue during recovery, there are situations where it may signal a more serious problem. Patients should be aware of the following warning signs that may require medical attention:

- Severe Abdominal Pain: If bloating is accompanied by intense abdominal pain or cramping that worsens over time, it may be a sign of an underlying complication, such as an infection or bowel obstruction.
- Persistent Vomiting or Nausea: If bloating is accompanied by vomiting, nausea, or an inability to keep food down, it may indicate a problem with the digestive tract that requires further evaluation.
- Fever: A fever may be a sign of infection, and if bloating is accompanied by a fever, it is essential to seek medical care immediately.
- Inability to Pass Gas or Stool: If bloating is accompanied by an inability to pass gas or have a bowel movement, it may suggest a more severe complication, such as a bowel obstruction. This situation requires prompt medical intervention.
Bloating is a common and often temporary symptom following an appendectomy. While it can be uncomfortable, it is typically manageable with the right care and attention. By understanding the causes of bloating and implementing preventative strategies, patients can reduce discomfort and promote a smoother recovery. Adopting good post-operative care practices, including early mobilization, dietary adjustments, and proper pain management, is key to minimizing bloating and facilitating optimal healing. If symptoms persist or worsen, it is essential to consult with a healthcare provider to rule out any complications.
With the right approach and proactive measures, most patients will find that bloating gradually diminishes as their body heals, allowing them to return to normal activities and enjoy a healthy recovery.