1. Understanding the Role of Vessels in Soft Tissue Cancer Surgery
A. Importance of Vascular Structures in Soft Tissue Sarcomas
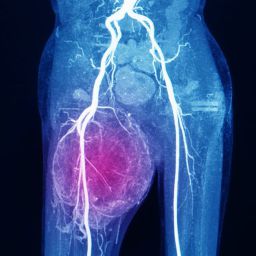
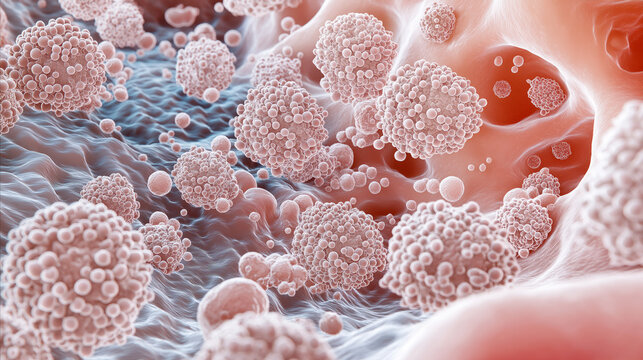
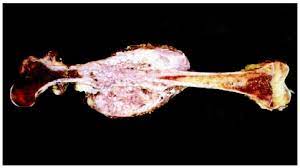
Soft tissue sarcomas can occur in any of the body’s soft tissues, many of which are richly vascularized. Vascular structures, including veins and arteries, are crucial for delivering oxygen and nutrients to tissues, and their proximity to tumors makes them vulnerable during surgery. The presence of large blood vessels near tumors complicates surgical procedures, as excessive bleeding during tumor excision can lead to life-threatening situations and impact surgical outcomes.
The close association between tumors and blood vessels means that removal of the tumor may necessitate cutting through or around important blood vessels. Surgeons must take great care to avoid damage to these vessels to prevent significant bleeding, which could compromise both the success of the operation and the patient’s recovery.
B. Vascular Blockage During Soft Tissue Cancer Surgery
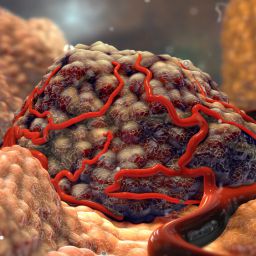
In addition to bleeding, vascular blockage can occur as a result of the surgery itself or as a complication of the tumor’s growth. Soft tissue sarcomas can invade blood vessels, leading to partial or complete obstruction. The removal of a tumor that involves the vascular system may lead to disruption of blood flow, which can result in ischemia (reduced blood supply) to surrounding tissues or organs.
When vascular blockage occurs, it can significantly affect the healing process, increase the risk of infection, and impact the functionality of the affected organ. In some cases, vascular blockage can even lead to the need for additional surgical interventions, such as bypass procedures or grafting to restore blood flow to the affected area.
2. Risks of Bleeding in Soft Tissue Cancer Surgery
Bleeding is one of the most common complications during soft tissue sarcoma surgeries, particularly when tumors are located in regions with a rich vascular supply, such as the limbs, abdomen, or retroperitoneum. Understanding the risk factors for bleeding and how to manage them is crucial for ensuring patient safety and optimizing surgical outcomes.
A. Causes of Bleeding in Soft Tissue Cancer Surgery
Several factors can contribute to bleeding during soft tissue sarcoma surgery:
- Tumor Size and Location: Large tumors or tumors located near major blood vessels have a higher risk of causing bleeding. For example, tumors in the pelvic area or abdomen may involve significant blood vessels, making surgical removal more challenging.
- Invasion of Blood Vessels: Many soft tissue sarcomas invade blood vessels, which can make it difficult to remove the tumor without damaging these vessels. If the blood vessels cannot be adequately repaired during surgery, excessive bleeding may occur.
- Poor Tumor Resectability: Some tumors may not be easily removed without incurring damage to blood vessels. In such cases, surgeons must carefully balance tumor excision with the risk of major bleeding.
B. Impact of Bleeding on Surgery and Recovery
Excessive bleeding during surgery can have a variety of negative consequences for the patient:
- Hemodynamic Instability: Profuse bleeding can lead to a significant drop in blood pressure, causing hemodynamic instability. This can result in shock, which is a life-threatening condition.
- Transfusion Requirements: Excessive blood loss may require blood transfusions, which carry risks, such as allergic reactions or transmission of infections.
- Increased Risk of Infection: Significant bleeding can disrupt normal tissue healing and increase the risk of infection at the surgical site. Infected surgical wounds can delay recovery and require additional treatments.
- Longer Recovery Time: Bleeding may extend the length of surgery, increase postoperative pain, and prolong the patient’s recovery time. It can also result in a longer hospital stay.
3. Preventive Measures for Vascular Blockage and Bleeding
While vascular blockage and bleeding are inherent risks during soft tissue cancer surgery, there are several strategies that surgeons can employ to minimize these risks and ensure the safety and well-being of patients.
A. Preoperative Planning
Preoperative planning is essential in reducing the risk of bleeding and vascular damage during surgery. Several steps can be taken before the surgery to anticipate potential challenges:
- Imaging Studies: Advanced imaging techniques, such as MRI, CT scans, and angiography, are invaluable for visualizing the tumor and its relationship to surrounding blood vessels. By identifying the size and location of blood vessels, surgeons can plan their approach and minimize the risk of inadvertent injury.
- Tumor Biopsy: A preoperative biopsy allows the surgical team to assess the tumor’s characteristics, including its proximity to blood vessels. This helps determine whether neoadjuvant therapies (e.g., radiation or chemotherapy) are needed to shrink the tumor before surgery.
- Blood Volume Optimization: Patients undergoing surgery for soft tissue sarcoma should be assessed for any underlying conditions that could increase the risk of bleeding, such as blood clotting disorders or low platelet counts. Blood volume and clotting function should be optimized before surgery to minimize bleeding risks.
B. Intraoperative Strategies for Minimizing Bleeding
During surgery, various techniques can be used to control bleeding and manage vascular risks:
- Hemostatic Techniques: Surgeons may use various hemostatic techniques, such as cauterization, ligation, or suturing, to control bleeding during the surgery. Electrocautery or laser technology can be employed to seal blood vessels and minimize the risk of bleeding.
- Vascular Clamping: Temporary clamping of major blood vessels may be necessary during tumor resection to minimize blood flow to the area. Once the tumor is removed, the clamp can be released, and blood flow can be restored.
- Intraoperative Monitoring: Continuous monitoring of vital signs, including blood pressure and heart rate, is essential during surgery. Monitoring can help detect early signs of bleeding or other complications, allowing for prompt intervention.
C. Postoperative Care and Monitoring
Even with the best surgical techniques, the risk of bleeding and vascular blockage remains postoperatively. Therefore, close monitoring and proactive care are crucial for a successful recovery:
- Drainage Systems: After surgery, drainage systems may be placed to remove excess fluid or blood from the surgical site. This helps prevent the accumulation of blood and reduces the risk of hematoma formation.
- Close Observation: Patients should be closely monitored for signs of excessive bleeding, such as a drop in blood pressure, increased heart rate, or swelling at the surgical site. Early intervention can prevent serious complications.
- Managing Blood Loss: In cases where bleeding does occur postoperatively, blood transfusions may be required to replace lost blood. The medical team should be prepared to respond quickly and appropriately.
- Physical Rehabilitation: Postoperative physical therapy can help improve circulation and reduce the risk of blood clots, which may contribute to vascular blockage in the postoperative period.
4. Potential Complications and Challenges
While preventive measures can significantly reduce the risk of vascular blockage and bleeding, some challenges remain. These may include:
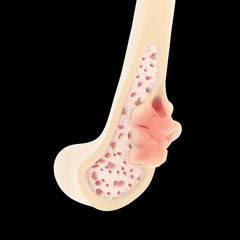
- Difficult Tumor Locations: Tumors located in complex anatomical areas, such as the pelvis or abdomen, may present significant challenges in both resection and vascular management.
- Tumor Recurrence: In cases of tumor recurrence, surgical challenges may increase due to the presence of scar tissue, adhesions, and altered blood vessel anatomy.
- Comorbid Conditions: Patients with other underlying health conditions, such as cardiovascular disease or diabetes, may face additional challenges in managing vascular risks during surgery.
Surgical intervention for soft tissue cancer presents significant challenges, particularly when dealing with vascular structures. The risks of vascular blockage and bleeding are major concerns that can complicate surgery and affect patient outcomes. However, with careful preoperative planning, advanced surgical techniques, and effective postoperative monitoring, the risks of bleeding and vascular complications can be minimized. Surgeons, working in collaboration with a multidisciplinary team, play a crucial role in ensuring that these risks are managed effectively to achieve the best possible outcomes for patients with soft tissue sarcoma.