1. Understanding Anal Fistulas and Their Treatment
Before addressing the risks of recurrence, it is important to understand the nature of anal fistulas and the common methods of treatment.
What Is an Anal Fistula?
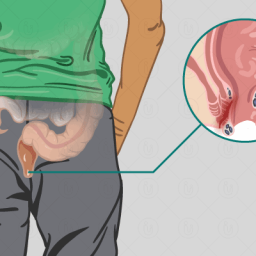
An anal fistula is a small tunnel that forms between the anal canal and the surrounding skin, often following an infection of the anal glands. These infections, which can become abscesses, cause inflammation and sometimes abscess drainage. If the abscess fails to heal properly, it may turn into a fistula.
Fistulas can be classified based on their location, size, and complexity. A simple anal fistula involves one tract and has minimal surrounding tissue involvement, while a complex anal fistula may have multiple tracts, involve deeper structures, and be more difficult to treat.
Treatment of Anal Fistulas
Treatment for anal fistulas typically involves surgical intervention. The primary goals are to:
- Drain any infection
- Close the fistula permanently
- Preserve sphincter function to avoid incontinence
Common surgical procedures for treating anal fistulas include:
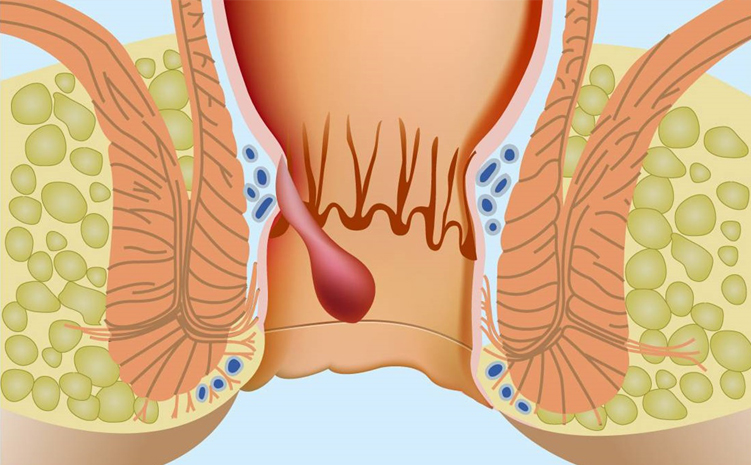
- Fistulotomy: The most common surgery for simple anal fistulas. The fistula is cut open to allow it to heal from the inside out.
- Seton Placement: A surgical thread is placed through the fistula to drain infection and help the fistula heal gradually.
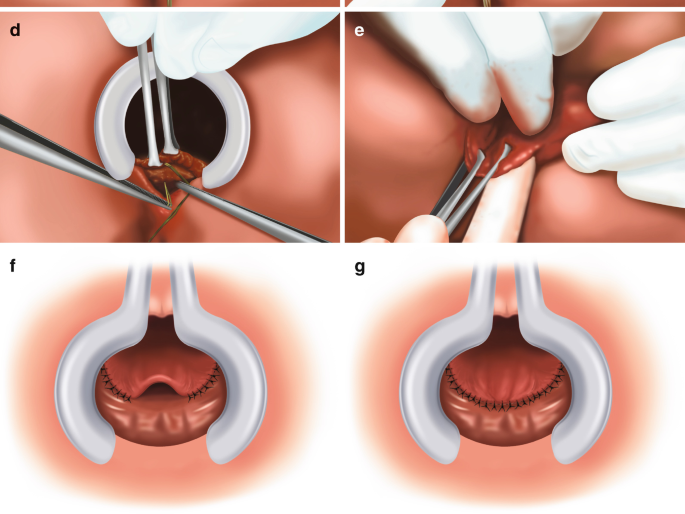
- Flap Repair: Used for more complex fistulas, this procedure involves closing the fistula with a piece of tissue from another part of the body.
- Ligation of the Intersphincteric Fistula Tract (LIFT): A technique where the fistula is dissected and ligated to prevent further drainage.
Although surgical treatments are generally effective, the risk of recurrence remains high in some cases. The treatment plan and recovery process depend on the complexity of the fistula and the overall health of the patient.
2. What Contributes to Anal Fistula Recurrence?
The risk of recurrence after anal fistula treatment can be attributed to various factors, ranging from the complexity of the fistula itself to the patient’s overall health and lifestyle choices. Several key elements contribute to the likelihood of a fistula returning after treatment:
Fistula Complexity
The complexity of the anal fistula is a significant factor in the likelihood of recurrence. Complex fistulas, which involve multiple tracts, cross the anal sphincter, or are associated with other conditions like Crohn’s disease, are more likely to recur. These fistulas are harder to treat and often require more advanced surgical interventions.
In contrast, simple anal fistulas with a single tract and no associated health complications have a higher success rate for complete healing after surgery. However, even simple fistulas can recur if not treated properly.
Inadequate Surgical Technique
The skill and experience of the surgeon play a critical role in the outcome of anal fistula surgery. Incomplete fistula removal, insufficient drainage, or improper closure of the fistula tract can increase the risk of recurrence. Additionally, if the surgical approach does not adequately preserve sphincter function or promote healing, a recurrence can occur.
Underlying Health Conditions
Certain health conditions increase the risk of anal fistula recurrence. Chronic inflammatory conditions such as Crohn’s disease and ulcerative colitis, as well as immunosuppressive conditions, can cause delayed healing or prevent the fistula from closing entirely. Patients with these conditions often experience repeated flare-ups of inflammation, which may cause the fistula to reopen.
Additionally, patients with diabetes, obesity, or other metabolic disorders may have a weakened immune response, making it more difficult for their bodies to heal effectively after surgery.
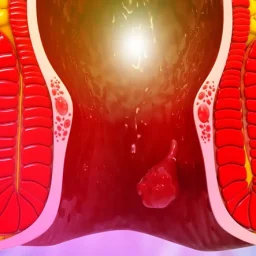
Infection and Abscess Formation
After surgery, an infection at the surgical site or within the fistula tract can lead to a recurrence of the fistula. Infection can prevent the healing process from proceeding as expected, causing complications such as abscess formation. This can reinstate the symptoms of the original fistula and create a need for further treatment or additional surgeries.
Lifestyle Factors
Certain lifestyle factors, such as poor hygiene, inadequate wound care, or physical strain, can also contribute to the recurrence of an anal fistula. Activities that increase pressure in the anal region, such as heavy lifting, can reopen the fistula tract or cause new fistulas to form. Additionally, smoking has been shown to hinder the healing process, reducing the effectiveness of surgical treatments.
3. What Should Be Considered After Treatment to Prevent Recurrence?
After treatment, a combination of medical management, lifestyle modifications, and ongoing care is necessary to reduce the risk of anal fistula recurrence. Patients need to understand their role in the recovery process and take steps to avoid situations that may promote the reappearance of the condition.

Post-Surgical Care and Hygiene
Maintaining proper hygiene and caring for the surgical site is crucial to prevent infection and recurrence. Patients should follow their surgeon’s post-operative instructions, which may include:
- Cleaning the area gently: Using mild, non-irritating soap and water to keep the area clean.
- Using sitz baths: Soaking the anal area in warm water can help soothe the site and reduce discomfort.
- Avoiding harsh chemicals or scented products: These can irritate the healing tissue and increase the risk of infection.
Regular follow-up visits with the surgeon or healthcare provider are necessary to monitor healing progress and detect any signs of recurrence early.
Dietary Modifications
A high-fiber diet is essential to promote regular bowel movements and reduce the risk of constipation, which can put strain on the anal area and potentially lead to the reformation of a fistula. Eating fiber-rich foods such as fruits, vegetables, and whole grains can help maintain soft stools and prevent trauma to the area during bowel movements.
For some patients, additional stool softeners may be prescribed to ensure that bowel movements remain comfortable and low-pressure.
Managing Underlying Conditions
Patients with underlying conditions like Crohn’s disease, diabetes, or inflammatory bowel disease must manage these conditions effectively to reduce the risk of fistula recurrence. This may include:
- Medications: Anti-inflammatory medications, immunosuppressants, or biologics to control inflammatory conditions.
- Regular monitoring: Ongoing management and monitoring by specialists (e.g., gastroenterologists) can help address flare-ups or complications before they impact the healing of the anal fistula.
4. Regular Follow-Up and Early Detection
Post-treatment follow-up appointments with a healthcare provider are critical for identifying potential complications or early signs of recurrence. These visits may involve physical examinations and imaging tests to ensure that the fistula has healed properly and that no new fistula formations are present.
Patients should be vigilant about monitoring their symptoms and seeking immediate medical attention if they notice any signs of infection, such as increased pain, swelling, redness, or discharge at the surgical site. Early intervention can prevent recurrence from becoming a more severe issue.
The Role of Surgery and Advanced Treatments in Preventing Recurrence
For patients with complex or recurrent anal fistulas, advanced surgical options may be necessary. These may include:
- Laser Fistula Treatment: A minimally invasive technique that uses laser energy to close the fistula tract.
- Fibrin Glue or Biologic Sealants: These materials can be injected into the fistula tract to help seal it and prevent further drainage.
- Stoma or Colostomy: In severe cases, the patient may need a temporary colostomy to give the anal area time to heal and prevent further trauma to the fistula site.
The success of these treatments depends on the complexity of the fistula and the patient’s overall health. In many cases, a combination of treatments may be necessary to achieve long-term success.
5. What Are the Psychological Impacts of Recurrence?
The recurrence of an anal fistula can have psychological effects on patients. Chronic pain, discomfort, and the need for additional treatments can be emotionally taxing. Many patients experience frustration, anxiety, or even depression when a fistula returns, particularly if they have undergone surgery with the expectation that the condition would be resolved.
Support from healthcare providers, family, and friends can help patients cope with the emotional challenges of recurrence. In some cases, patients may benefit from counseling or therapy to address feelings of anxiety, frustration, or embarrassment related to the condition.
While the surgical treatment of anal fistulas is often effective, the risk of recurrence remains an important concern. Understanding the factors that contribute to recurrence, such as the complexity of the fistula, surgical technique, underlying health conditions, and lifestyle factors, is crucial for both patients and healthcare providers. By taking preventive measures, including proper post-operative care, managing underlying health conditions, and adhering to follow-up schedules, the risk of recurrence can be minimized. However, even with the best care, some patients may face the challenge of dealing with recurrent fistulas. Through early detection and ongoing management, the impact of anal fistula recurrence can be managed, improving patients’ quality of life and outcomes