1. Primary Liver Cancer
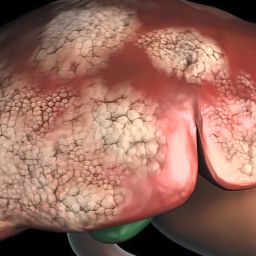
Primary liver cancer refers to cancers that begin in the liver itself. The majority of liver cancers fall into this category, with hepatocellular carcinoma (HCC) being by far the most common type. However, other types of primary liver cancer, including intrahepatic cholangiocarcinoma and hepatoblastoma, also exist. Primary liver cancer is typically associated with chronic liver diseases such as cirrhosis, hepatitis B and C infections, and non-alcoholic fatty liver disease (NAFLD).
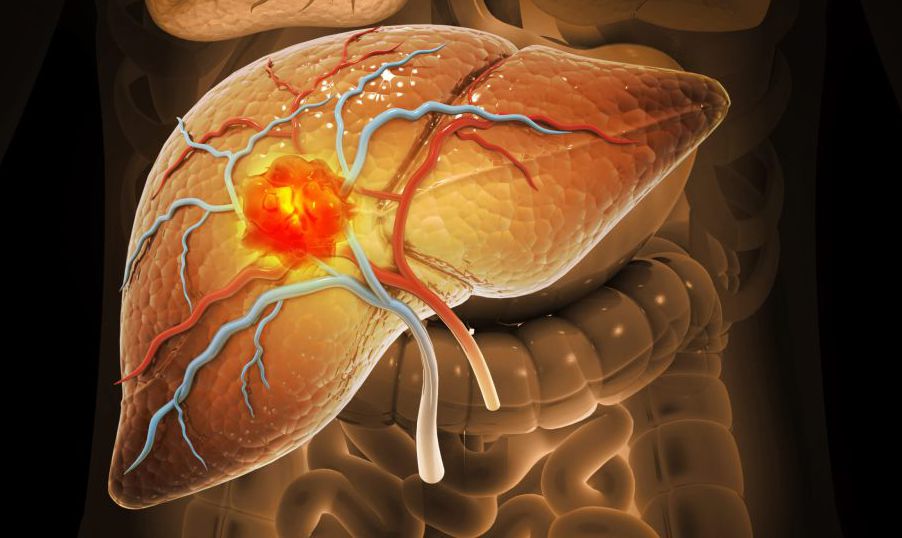
1.1 Hepatocellular Carcinoma (HCC)
Hepatocellular carcinoma (HCC) is by far the most common and aggressive form of liver cancer, accounting for approximately 75% of all primary liver cancers. It originates from hepatocytes, the main functional cells of the liver.
Risk Factors:
HCC is strongly associated with chronic liver diseases. The most common risk factors include:
- Chronic viral infections such as hepatitis B (HBV) and hepatitis C (HCV)
- Cirrhosis, often caused by chronic alcohol abuse or NAFLD
- Aflatoxin exposure from contaminated food
- Genetic conditions such as hereditary hemochromatosis
Symptoms:
In its early stages, HCC may not present any noticeable symptoms. As the tumor grows, symptoms can include abdominal pain, weight loss, jaundice (yellowing of the skin and eyes), fatigue, and swelling in the abdomen due to fluid accumulation (ascites).

Diagnosis and Treatment:
HCC is typically diagnosed through imaging tests like ultrasound, CT scans, or MRI, along with blood tests to check for elevated levels of liver enzymes and alpha-fetoprotein (AFP), a protein often elevated in HCC cases. Treatment options for HCC vary depending on the tumor’s size, location, and the extent of liver damage. These options include:
- Surgical resection (removal of the tumor)
- Liver transplantation
- Ablation therapies (such as radiofrequency or microwave ablation)
- Chemotherapy and targeted therapies
- Immunotherapy
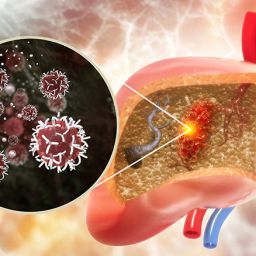
1.2 Intrahepatic Cholangiocarcinoma (ICC)
Intrahepatic cholangiocarcinoma (ICC) is the second most common type of primary liver cancer. It originates in the bile ducts that are located within the liver, specifically the small bile ducts. ICC is less common than HCC but has become more frequently diagnosed in recent years.
Risk Factors:
Several risk factors contribute to the development of ICC, including:
- Chronic liver diseases such as primary sclerosing cholangitis (PSC)
- Chronic viral infections like hepatitis B or C
- Exposure to certain chemicals, including industrial solvents
- Liver fluke infections, particularly in parts of Asia
- Liver cirrhosis or NAFLD
Symptoms:
The symptoms of ICC are often nonspecific and can overlap with those of other liver diseases. Common symptoms include jaundice, abdominal pain, unintentional weight loss, and fever. Because ICC is often diagnosed at an advanced stage, it can be more challenging to treat effectively.
Diagnosis and Treatment:
The diagnosis of ICC is typically confirmed using imaging tests such as CT scans, MRIs, and liver biopsy. Tumor markers like CA 19-9 are also used in diagnosis. Treatment options for ICC are often limited, and surgical resection is only possible in a small proportion of patients. If surgery is not an option, other treatments include:
- Chemotherapy
- Liver transplantation
- Palliative care to manage symptoms
1.3 Hepatoblastoma
Hepatoblastoma is a rare type of liver cancer that primarily affects children, particularly those under the age of 3. It originates in the liver’s precursor cells, known as hepatoblasts. Although hepatoblastoma is rare, it is the most common type of liver cancer in infants and children.
Risk Factors:
The exact cause of hepatoblastoma is not fully understood, but several risk factors have been identified:
- Genetic disorders such as Beckwith-Wiedemann syndrome
- Premature birth and low birth weight
- Familial adenomatous polyposis (FAP)
Symptoms:
In children, hepatoblastoma often presents with abdominal swelling, pain, and an abdominal mass. Other symptoms may include poor growth, weight loss, and jaundice.
Diagnosis and Treatment:
Diagnosis is made using imaging techniques like ultrasound, CT, or MRI, along with blood tests to assess AFP levels. Treatment typically involves surgery to remove the tumor, and chemotherapy is often used in conjunction with surgery. Hepatoblastoma has a relatively good prognosis when treated promptly and aggressively.
2. Secondary Liver Cancer
Secondary liver cancer, also called metastatic liver cancer, refers to cancer that has spread (metastasized) from other organs to the liver. This is far more common than primary liver cancer, and most cases of liver cancer are secondary cancers. Cancers from other organs such as the colon, pancreas, breast, and lungs frequently spread to the liver.
2.1 Colorectal Cancer Metastasis
Colorectal cancer is one of the most common cancers to metastasize to the liver. The liver is the first organ to receive blood from the intestines, which is why it is a frequent site of metastasis for colorectal cancer cells.
Risk Factors:
The risk factors for colorectal cancer include a family history of colorectal cancer, inflammatory bowel disease (such as Crohn’s disease or ulcerative colitis), a sedentary lifestyle, a high-fat diet, and age (people over 50 are at higher risk).
Symptoms and Diagnosis:
Symptoms of metastatic colorectal cancer in the liver include jaundice, abdominal pain, nausea, and weight loss. Diagnosis is made through imaging techniques like CT scans and MRIs, alongside biopsy and blood tests for tumor markers like CEA (carcinoembryonic antigen).
Treatment:
Treatment for liver metastasis from colorectal cancer often includes a combination of chemotherapy, surgery to remove the liver tumor, and sometimes liver-directed therapies such as radiofrequency ablation. Liver transplantation is rarely an option for metastatic colorectal cancer.
2.2 Other Common Metastatic Cancers
In addition to colorectal cancer, other cancers that commonly spread to the liver include:
- Breast Cancer: Metastatic breast cancer to the liver often occurs when the cancer cells spread through the bloodstream. Treatment for breast cancer liver metastasis usually involves chemotherapy, targeted therapies, and sometimes liver resection.
- Lung Cancer: Lung cancer, particularly non-small cell lung cancer, can metastasize to the liver, often in the later stages of the disease. Treatment typically includes chemotherapy, targeted therapy, and palliative care.
- Pancreatic Cancer: Pancreatic cancer commonly spreads to the liver due to its proximity and the liver’s role in filtering blood. Treatment usually involves chemotherapy and palliative care.
3. Risk Factors for Liver Cancer
Understanding the various risk factors for liver cancer, including those for primary and secondary liver cancer, can help in the early detection and prevention of the disease. Key risk factors include:
- Chronic liver disease (especially hepatitis B and C infections)
- Cirrhosis
- Alcohol consumption
- Obesity and diabetes
- Exposure to aflatoxins
- Genetic conditions like hereditary hemochromatosis
4. Prevention and Early Detection
Liver cancer, particularly HCC, is often preventable or manageable if caught early. Preventive measures include:
- Vaccination against hepatitis B
- Antiviral treatments for hepatitis B and C
- Alcohol moderation
- Weight management and diabetes control
- Regular screenings for individuals at high risk (those with chronic liver disease)
Early detection through regular screening, including imaging tests and blood tests for liver function and tumor markers like AFP, is critical for improving prognosis.
Liver cancer is a complex disease with several types, each with distinct characteristics and treatment approaches. Hepatocellular carcinoma remains the most common form of liver cancer, but intrahepatic cholangiocarcinoma and hepatoblastoma also play significant roles. Secondary liver cancers, particularly from colorectal, breast, and lung cancers, are far more common than primary liver cancers.
Understanding the types of liver cancer and their risk factors is vital for early detection and treatment. As research advances, there is hope for more targeted therapies and improved survival rates for liver cancer patients.