1. The Role of the Spleen in the Immune System
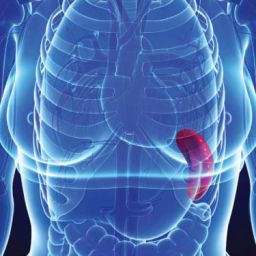
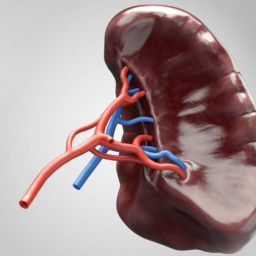
Before diving into the changes following splenectomy, it is essential to understand the spleen’s primary function in the immune system. The spleen is located on the left side of the abdomen, near the stomach, and acts as a filter for the blood. It removes old or damaged red blood cells and platelets, recycling iron, and it plays a role in the production of certain white blood cells that are vital to the body’s immune response. The spleen is rich in lymphocytes—particularly B and T cells—which help the body recognize and fight pathogens like bacteria, viruses, and parasites.
Additionally, the spleen stores a large amount of monocytes, which are a type of white blood cell that helps fight infections. When the body is exposed to infection, the spleen releases monocytes into the bloodstream to help control the immune response.
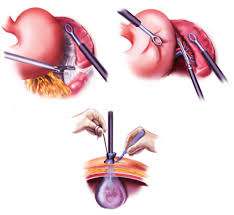
Given this crucial role in immunity, the removal of the spleen (splenectomy) necessitates significant adjustments to the immune system, requiring the body to adapt in several ways.
2. Immediate Impact on Immune Function After Splenectomy
The immediate impact of splenectomy on the immune system is significant. Without a spleen, the body loses one of its most important organs in filtering and fighting infections. However, while the body compensates in various ways, the loss of the spleen leads to an increased vulnerability to certain types of infections, particularly those caused by encapsulated bacteria.

a. Increased Susceptibility to Infections
One of the most critical effects of splenectomy is an increased susceptibility to infections, particularly bacterial infections caused by organisms that form protective capsules around themselves. These bacteria, including Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis, are normally targeted and removed by the spleen. After splenectomy, the body’s ability to clear these bacteria is reduced, leading to a higher risk of severe infections, particularly pneumonia, meningitis, and sepsis.
b. Reduced Immune Response to Blood-Borne Pathogens
The spleen is vital for filtering blood-borne pathogens, and without it, the body loses an essential line of defense. While other organs, such as the liver, may take over some of the spleen’s functions, the immune response is less efficient. For instance, the liver can filter out blood cells and help in clearing some pathogens, but it does not perform the specialized immune function of the spleen. As a result, the body may take longer to respond to infections, and the severity of infections can be greater.
3. Long-Term Effects on Immune Function
In the long term, the immune system adapts to the loss of the spleen, but the adaptations come with limitations. People who have undergone splenectomy must take proactive steps to reduce the risk of infections.
a. Immune System Adaptation
While the spleen is an important immune organ, other components of the immune system can adapt to fill the void left by the spleen’s removal. The bone marrow, lymph nodes, and liver play more prominent roles in filtering the blood and fighting infections after splenectomy. Over time, other organs may increase the production of certain immune cells that were previously generated by the spleen, such as monocytes and some types of lymphocytes. However, these organs do not fully replace the spleen’s specific functions in immune regulation.
b. Vaccination and Prophylactic Antibiotics
To help compensate for the loss of the spleen, patients who undergo splenectomy are often recommended to receive vaccinations and prophylactic antibiotics. Vaccines such as the pneumococcal vaccine, meningococcal vaccine, and Haemophilus influenzae type b vaccine are crucial in preventing infections. These vaccines help reduce the risk of serious bacterial infections by stimulating the immune system to recognize and fight off specific pathogens.
Prophylactic antibiotics may also be prescribed for individuals who have had their spleen removed, particularly in the immediate post-surgical period or during times of high risk, such as after an illness or infection. These antibiotics provide additional protection against infections while the immune system adapts to the change.
c. Increased Risk of Sepsis
One of the most dangerous complications after splenectomy is the increased risk of sepsis, a life-threatening infection that can spread throughout the body. Since the spleen plays a vital role in filtering and removing harmful pathogens, its removal means that the body may not respond to infections as quickly or as effectively. This increased vulnerability to infections makes it crucial for splenectomy patients to be vigilant about any signs of infection and seek prompt medical care if they develop symptoms like fever, chills, or difficulty breathing.
4. Potential for Autoimmune Responses and Blood Disorders
Interestingly, splenectomy can also have an impact on other aspects of the immune system, such as autoimmune responses and blood health.
a. Autoimmune Responses
While the immune system adapts to the loss of the spleen, it can also lead to changes in immune function that predispose some individuals to autoimmune diseases. The spleen helps regulate immune tolerance, and without it, the body may be more prone to attacks on its own cells and tissues. For example, patients who undergo splenectomy may be at an increased risk of developing autoimmune conditions such as rheumatoid arthritis or lupus, although this risk is relatively low.
b. Blood Disorders
The spleen is responsible for breaking down old red blood cells and platelets. After splenectomy, other organs, such as the liver, may take on this responsibility, but they do so less efficiently. This can lead to changes in the blood count, and in some cases, the development of blood disorders such as thrombocytosis (high platelet count) or anemia. These blood disorders often require ongoing medical management, including regular blood tests and sometimes medication to help regulate blood cell production.
5. Lifestyle Adjustments and Ongoing Care
Individuals who have had a splenectomy must make certain lifestyle adjustments to ensure their long-term health and well-being. Beyond vaccinations and antibiotic therapy, these patients should adopt practices that help minimize the risk of infections. This includes regular check-ups with their healthcare providers, early intervention if any signs of infection occur, and avoiding situations where infections are more likely, such as crowded public spaces during flu season.
Patients should also carry medical identification to inform healthcare professionals of their splenectomy, as this can help guide treatment decisions in case of an emergency.
The removal of the spleen is a significant procedure that affects many aspects of the body’s functioning, particularly the immune system. While the immune system can adapt over time, individuals who undergo splenectomy are at increased risk of infections, particularly those caused by encapsulated bacteria. By understanding the effects of splenectomy and taking appropriate precautions, such as vaccinations and antibiotic use, patients can better manage their health after surgery. The adaptation process is ongoing, and with proper medical care and vigilance, most individuals can lead healthy lives even without a spleen.