1. Clinical Presentation and Symptoms of GIST
The diagnosis of GIST often begins with recognizing the symptoms associated with the condition. However, because these symptoms are nonspecific and can overlap with other gastrointestinal disorders, a GIST may not be suspected until further testing is performed. Common symptoms include:
- Abdominal pain or discomfort
- Bloating or a sense of fullness
- Difficulty swallowing (if the tumor is located in the esophagus or upper stomach)
- Unexplained weight loss
- Gastrointestinal bleeding (resulting in black stools or vomiting blood)
- Anemia (due to chronic blood loss)
In some cases, patients may not experience noticeable symptoms until the tumor reaches a considerable size. This is why regular medical check-ups and early imaging tests are essential for individuals at higher risk or those experiencing persistent symptoms.
2. Medical History and Physical Examination
Before diving into specific tests, a physician will conduct a thorough medical history and physical examination. During the physical exam, a doctor may detect a palpable mass in the abdomen or other signs of a gastrointestinal issue. They may also inquire about the patient’s family history, lifestyle, and any risk factors, such as previous gastrointestinal conditions, prior surgeries, or inherited disorders.
Importance of Medical History:
- Risk Factors: Patients with certain genetic conditions, such as Neurofibromatosis Type 1 (NF1) or Carney-Stratakis syndrome, are at an increased risk of developing GIST. These conditions should be considered when evaluating the patient’s medical history.
- Symptoms Review: A detailed review of symptoms helps doctors decide which diagnostic tests to prioritize based on clinical presentation.
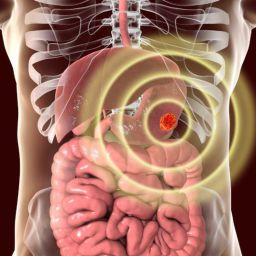
3. Imaging Tests for GIST Diagnosis
Imaging techniques are fundamental in diagnosing GISTs. These tests allow doctors to visualize the size, location, and characteristics of the tumor. Different types of imaging may be used to identify suspicious masses, assess the tumor’s impact on surrounding tissues, and guide biopsy procedures.
a. Ultrasound (Abdominal Ultrasound)
- Overview: An abdominal ultrasound can sometimes detect a GIST, especially when the tumor is large. This technique uses high-frequency sound waves to create an image of the internal organs. While ultrasound is a non-invasive procedure, it is generally not the primary tool for diagnosing GIST, as it can be difficult to assess the tumor’s precise location or characteristics.
- Limitations: An ultrasound may not offer enough detail or precision for definitive diagnosis, especially if the tumor is deep within the tissue.
b. Computed Tomography (CT) Scan
- Overview: A CT scan, often enhanced with contrast agents, is one of the most commonly used imaging techniques for detecting GISTs. It provides detailed cross-sectional images of the abdomen and can help identify tumors, their size, and their location within the GI tract.
- Benefits: CT scans can also provide important information about the tumor’s potential spread (metastasis) to other organs or nearby lymph nodes. This is critical for determining the stage of the cancer.
- Contrast-Enhanced CT: The use of a contrast agent during the CT scan enhances the visibility of blood vessels, allowing doctors to evaluate blood flow to the tumor and assess any potential internal bleeding or vessel invasion by the tumor.
c. Magnetic Resonance Imaging (MRI)
- Overview: MRI scans provide high-resolution images and can help identify soft tissue tumors. This imaging method can be particularly useful for evaluating tumors in areas where CT scans may be less effective, such as in the pelvis or areas with overlapping structures.
- Benefits: MRI is non-invasive and does not use radiation. It is typically employed when additional details about the tumor’s size, location, or surrounding structures are needed.
- Limitations: MRI is generally more time-consuming and less accessible than CT scans.
d. Positron Emission Tomography (PET) Scan
- Overview: A PET scan can be used in conjunction with CT scans (known as PET-CT) to assess the metabolic activity of a tumor. Cancer cells typically have a higher metabolic rate than normal cells, and PET scans can detect areas of increased activity, helping to identify tumors and assess whether the cancer has spread to other parts of the body.
- Benefits: PET scans are particularly useful for detecting metastasis and monitoring treatment response in patients with known GIST.
- Limitations: PET scans may not always detect small tumors and are usually not the first imaging technique used in GIST diagnosis.
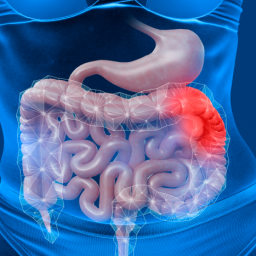
4. Endoscopy
Endoscopy plays a vital role in the diagnosis and management of GISTs, particularly when the tumor is located in the upper gastrointestinal tract or near the stomach or intestines. Endoscopic procedures involve the use of a flexible tube with a camera at the tip, allowing the physician to visualize the inside of the gastrointestinal tract.

a. Esophagogastroduodenoscopy (EGD)
- Overview: EGD, also known as an upper endoscopy, involves inserting a flexible scope through the mouth to examine the esophagus, stomach, and duodenum (the first part of the small intestine). It can detect the presence of tumors in these regions and help doctors determine the tumor’s size and shape.
- Benefits: EGD is minimally invasive, providing direct visualization of the tumor. It is also useful in cases where the tumor is causing gastrointestinal bleeding or difficulty swallowing.
- Limitations: While EGD can identify the tumor, it does not provide detailed information about the tissue’s nature or allow for a definitive diagnosis without a biopsy.
b. Endoscopic Ultrasound (EUS)
- Overview: EUS is an advanced form of endoscopy that combines ultrasound technology with a flexible endoscope. It provides high-resolution images of the tumor and can assess its relationship to nearby tissues.
- Benefits: EUS is particularly useful for evaluating tumors in the stomach and duodenum, where it can provide detailed images of the layers of the GI wall. It can also help guide biopsy procedures, allowing for the collection of tissue samples directly from the tumor.
- Limitations: EUS is not as effective for tumors in the colon or areas further along the GI tract.
5. Biopsy and Histopathological Examination
A definitive diagnosis of GIST requires a tissue sample, which is obtained through a biopsy. Biopsy is the process of extracting a small sample of tissue from the tumor for microscopic examination. There are several methods for obtaining a biopsy in suspected GIST cases:
a. Fine-Needle Aspiration (FNA)
- Overview: FNA involves using a thin, hollow needle to remove a small sample of tissue from the tumor. This procedure can be done under imaging guidance, such as ultrasound or CT scans, to target the tumor.
- Benefits: FNA is a minimally invasive procedure that allows for rapid collection of tissue for analysis. It is often used when the tumor is accessible from the skin or during endoscopic procedures.
- Limitations: FNA may not always provide a sufficient amount of tissue for diagnosis, and additional biopsy methods may be needed.
b. Core Needle Biopsy
- Overview: A core needle biopsy removes a larger tissue sample compared to FNA. It is typically used when a more substantial tissue sample is needed to evaluate the tumor’s structure and cellular makeup.
- Benefits: This method provides more tissue for pathological examination, making it easier to assess the tumor’s characteristics.
- Limitations: It is more invasive than FNA and may require local anesthesia.
6. Molecular Testing for GIST
After obtaining a tissue sample, molecular testing plays a key role in confirming a diagnosis of GIST and determining the most appropriate treatment approach.
a. Immunohistochemistry (IHC)
- Overview: IHC is a laboratory technique that uses antibodies to detect specific proteins in the tumor cells. For GIST, the presence of the KIT protein (CD117) or PDGFRA protein is a key diagnostic marker.
- Benefits: A positive result for either KIT or PDGFRA mutations confirms the diagnosis of GIST and helps guide treatment decisions, especially regarding targeted therapies such as imatinib.
b. Genetic Testing
- Overview: GISTs are often associated with specific genetic mutations in the KIT or PDGFRA genes. Genetic testing can identify these mutations, which are critical for selecting targeted therapy.
- Benefits: Identifying the specific mutation enables doctors to prescribe targeted therapies that may improve treatment outcomes, as these therapies work by inhibiting the proteins produced by the mutated genes.
Diagnosing Gastrointestinal Stromal Tumors (GISTs) is a complex and multi-step process involving a combination of clinical evaluation, imaging studies, endoscopy, biopsy, and molecular testing. Early diagnosis is key to improving patient outcomes, as it allows for the timely initiation of appropriate treatments. Through the use of these advanced diagnostic methods, healthcare providers can confirm the presence of GIST, assess its stage, and develop a tailored treatment plan that increases the chances of successful management and improved quality of life for patients.