Thyroid Cancer is Always Fatal
One of the most pervasive myths about thyroid cancer is that it is always fatal. While any cancer diagnosis can be frightening, thyroid cancer is one of the most treatable forms of cancer, especially when caught early. According to the American Cancer Society, the 5-year survival rate for most types of thyroid cancer is very high, with some forms having survival rates exceeding 98%.
The prognosis depends on various factors, including the type of thyroid cancer, its stage at diagnosis, the patient’s age, and overall health. The majority of thyroid cancers, especially papillary and follicular thyroid cancers, are highly treatable, and many patients can live long, healthy lives following treatment. Even in cases where the cancer has spread to lymph nodes, survival rates remain high with proper treatment.
Only Older People Get Thyroid Cancer
Another common misconception is that thyroid cancer affects only older adults. While the average age of diagnosis is between 45 and 60, thyroid cancer can occur at any age. In fact, thyroid cancer is one of the most common cancers in young adults, especially in women under the age of 40.
Papillary thyroid cancer, the most common form of thyroid cancer, tends to affect younger women, while medullary and anaplastic thyroid cancers are more common in older adults. Additionally, thyroid cancer can be found in children, although it is rare. The key takeaway is that thyroid cancer is not age-exclusive, and it is important for people of all ages to be aware of the signs and symptoms, as early detection can significantly improve treatment outcomes.
A Lump in the Neck Always Means Thyroid Cancer

Finding a lump or nodule in the neck can understandably be alarming, but it is important to remember that most thyroid nodules are benign (non-cancerous). In fact, studies show that about 60-70% of adults have thyroid nodules, yet only a small percentage of these nodules are cancerous.
Thyroid nodules are common, and they may be detected during routine physical exams or imaging studies for other health issues. While some nodules may indeed turn out to be cancerous, the vast majority are harmless. It is important to have any lump or nodule evaluated by a healthcare professional, who can use various diagnostic tools, such as ultrasound and biopsy, to determine if further investigation is necessary.
Thyroid Cancer Symptoms are Obvious
Unlike some other types of cancer, thyroid cancer does not always cause noticeable symptoms, especially in the early stages. This is why it can often go undetected until it is more advanced. Common symptoms of thyroid cancer include a lump in the neck, difficulty swallowing or breathing, hoarseness, and pain in the neck or throat. However, these symptoms can also be caused by many other conditions, such as benign thyroid conditions, infections, or even allergies.
Because the symptoms are not always specific to thyroid cancer, routine screenings or regular visits to a healthcare provider are essential for those at higher risk. It is important to note that if thyroid cancer does cause symptoms, they tend to appear only as the cancer grows or spreads. This highlights the significance of early detection, which is often the key to successful treatment.
Thyroid Cancer Only Affects Women
Thyroid cancer is more common in women than men, but that does not mean it only affects women. Men can and do develop thyroid cancer, although the overall incidence is lower in men. The reasons behind this gender disparity are not fully understood but are believed to involve hormonal and genetic factors.
While women are more likely to develop papillary thyroid cancer, men are more likely to develop the more aggressive types of thyroid cancer, such as medullary and anaplastic thyroid cancer. Though it is less common, men tend to have poorer outcomes due to the more aggressive nature of these forms of the disease. Both men and women should be vigilant about their thyroid health and seek medical advice if they notice unusual symptoms.
Thyroid Cancer is Always a Result of Genetic Inheritance

While genetic factors can play a role in the development of thyroid cancer, the majority of cases are not inherited. In fact, most cases of thyroid cancer occur in people with no family history of the disease. Only a small percentage of thyroid cancer cases are due to inherited genetic mutations, such as those seen in familial medullary thyroid cancer or certain genetic syndromes like multiple endocrine neoplasia (MEN).
However, certain genetic mutations and family history may increase the risk of developing thyroid cancer. If someone has a close relative with thyroid cancer or a genetic condition known to increase the risk, they should discuss screening and monitoring options with their doctor. For the vast majority of thyroid cancer patients, lifestyle factors, environmental exposures, and chance play a more significant role than genetics.
Radiation Exposure is the Only Risk Factor for Thyroid Cancer
While radiation exposure is a well-known risk factor for thyroid cancer, it is not the only one. In fact, many people diagnosed with thyroid cancer have no known exposure to radiation. Other potential risk factors include:
- Gender: Women are more likely to develop thyroid cancer than men.
- Age: The risk of thyroid cancer increases with age, though it can affect younger individuals as well.
- Family history: A family history of thyroid cancer or certain genetic syndromes may increase risk.
- Iodine deficiency: In regions where iodine deficiency is common, thyroid cancer rates may be higher.
- Certain medical conditions: Having a history of other thyroid diseases, such as Hashimoto’s thyroiditis or goiter, can slightly increase the risk.
Thus, while radiation exposure (especially during childhood) is a significant risk factor, many individuals diagnosed with thyroid cancer do not have any obvious risk factors. This highlights the importance of awareness and vigilance for all individuals, regardless of their perceived risk.
Surgery is the Only Treatment for Thyroid Cancer
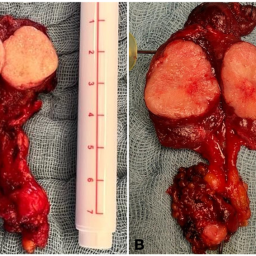
Surgery is the primary treatment for most cases of thyroid cancer, particularly for those with larger tumors or cancer that has spread to lymph nodes. However, it is not the only treatment option. Depending on the type and stage of thyroid cancer, other treatments may be used, either alone or in combination with surgery:

- Radioactive iodine therapy (RAI): After surgery, radioactive iodine may be used to destroy any remaining cancer cells. This treatment is especially effective for papillary and follicular thyroid cancers.
- Thyroid hormone therapy: Following surgery, patients may need to take thyroid hormone replacement medication to replace the thyroid hormone their body can no longer produce.
- External radiation therapy: In cases of anaplastic thyroid cancer or in certain situations where the cancer has spread, radiation therapy may be used.
- Chemotherapy: Chemotherapy is generally reserved for more advanced cases of thyroid cancer, particularly anaplastic thyroid cancer, as it is more aggressive and less responsive to other treatments.
The treatment plan is individualized based on the type, stage, and aggressiveness of the cancer. Advances in thyroid cancer treatment have led to better outcomes, and surgery remains a key element in treatment, but it is part of a comprehensive approach.
Thyroid Cancer Cannot Be Prevented
While there is no surefire way to prevent thyroid cancer, there are some steps individuals can take to reduce their risk. These include:
- Avoiding unnecessary radiation exposure: Limiting unnecessary exposure to radiation, especially during childhood, can reduce the risk of developing thyroid cancer later in life.
- Maintaining a healthy diet: Adequate intake of iodine is important for thyroid health. In areas where iodine deficiency is common, iodine supplements or iodized salt can help reduce the risk.
- Regular check-ups: People with a family history of thyroid cancer or those at increased risk should have regular check-ups and screenings to catch any early signs of thyroid issues.
While it is impossible to prevent every case of thyroid cancer, being proactive about thyroid health can help identify problems early and increase the likelihood of successful treatment.
Thyroid cancer is often misunderstood due to the prevalence of myths and misconceptions surrounding it. By addressing these myths and providing accurate information, we can foster a better understanding of the disease. Thyroid cancer is highly treatable, and early detection significantly improves the prognosis for most patients. While there is no foolproof way to prevent thyroid cancer, regular check-ups, a healthy lifestyle, and awareness of risk factors can help reduce the chances of developing the disease or catching it in its early stages. If you notice any changes in your neck or throat, it is essential to consult a healthcare professional to determine whether further evaluation is needed.