1. Common Causes of Rectal Bleeding
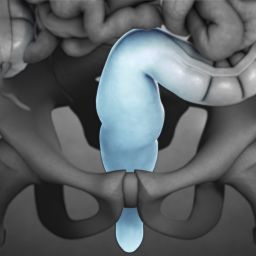
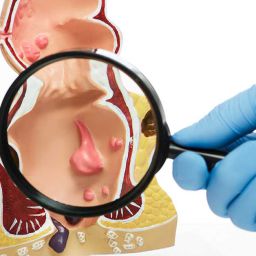
1.1 Hemorrhoids Hemorrhoids are swollen blood vessels in the anus or lower rectum, and they are one of the most common causes of rectal bleeding. They can be internal or external and cause symptoms such as itching, pain, and bright red blood on the stool or toilet paper. Hemorrhoids are often caused by straining during bowel movements, constipation, or prolonged sitting on the toilet.
1.2 Anal Fissures An anal fissure is a small tear in the skin around the anus, usually caused by passing hard stools. The tear can cause sharp pain during and after a bowel movement and may be accompanied by bright red blood. Anal fissures are more common in individuals who experience constipation or diarrhea.
1.3 Gastrointestinal Bleeding Bleeding from the upper gastrointestinal tract (such as the stomach, esophagus, or small intestine) can result in dark or tarry stools. Common causes of gastrointestinal bleeding include peptic ulcers, gastric erosions, or esophageal varices. This type of bleeding may not be immediately visible but can be detected through stool tests or endoscopy.
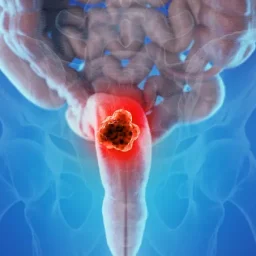
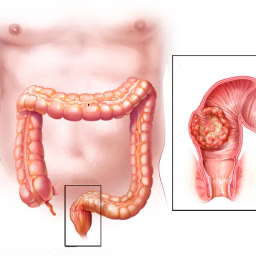
1.4 Colorectal Cancer Colorectal cancer can cause rectal bleeding, which may range from minor spotting to more significant blood loss. In early stages, blood in the stool may not be obvious, but as the cancer progresses, it may lead to visible bleeding. Colorectal cancer may also cause other symptoms such as changes in bowel habits, unexplained weight loss, and abdominal pain.
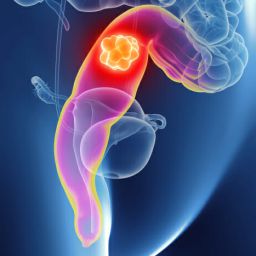
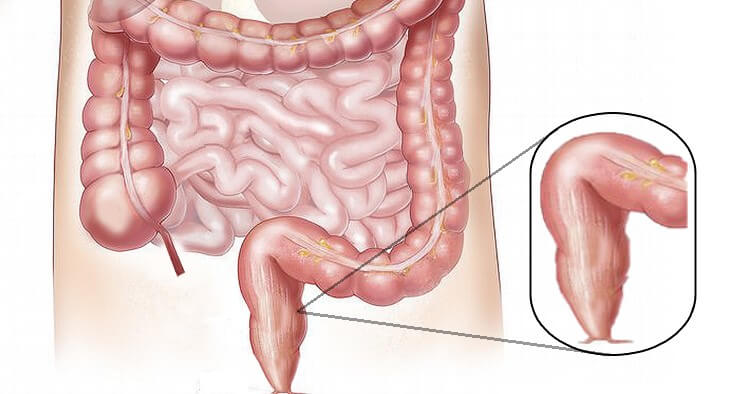
1.5 Diverticulosis and Diverticulitis Diverticulosis occurs when small pouches (diverticula) form in the wall of the colon. While most people with diverticulosis do not experience symptoms, in some cases, these pouches can become inflamed or infected (diverticulitis), leading to rectal bleeding. This bleeding may be significant and can result in bright red blood in the stool.
1.6 Inflammatory Bowel Disease (IBD) Inflammatory bowel diseases, such as Crohn’s disease and ulcerative colitis, can cause inflammation and ulcers in the digestive tract, leading to bleeding. Blood may appear in the stool, often accompanied by other symptoms such as diarrhea, abdominal cramps, and fatigue. IBD typically affects the colon and rectum but can affect any part of the gastrointestinal tract.
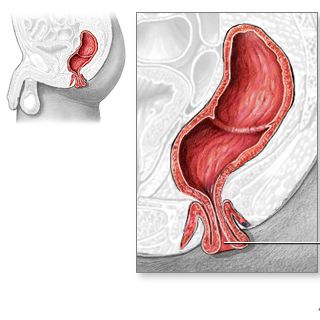
1.7 Rectal Prolapse Rectal prolapse occurs when part of the rectum protrudes from the anus, leading to discomfort and sometimes rectal bleeding. This condition can be associated with chronic constipation, pelvic floor weakness, and straining during bowel movements.
1.8 Other Causes Other potential causes of rectal bleeding include infections, such as sexually transmitted infections (STIs), and certain medications, such as blood thinners or nonsteroidal anti-inflammatory drugs (NSAIDs). These factors may contribute to rectal bleeding, particularly in individuals with underlying health conditions.
2. When Should You See a Doctor?
2.1 Severity of the Bleeding The amount and frequency of rectal bleeding can help determine whether medical attention is needed. A small amount of blood on the toilet paper or stool may not be a cause for concern, especially if the bleeding is intermittent. However, if you experience significant or continuous bleeding, it is important to consult a healthcare provider promptly.
2.2 Accompanying Symptoms If rectal bleeding is accompanied by other concerning symptoms, such as:
- Severe Abdominal Pain
- Unexplained Weight Loss
- Persistent Diarrhea
- Fatigue or Weakness
- Anemia (pale skin, shortness of breath)
It is important to seek medical advice immediately, as these symptoms may indicate a more serious condition, such as colorectal cancer or an inflammatory bowel disease (IBD).
2.3 Duration of Symptoms If the bleeding lasts more than a few days or recurs over time, it is essential to see a doctor. Persistent bleeding, especially when there are no obvious causes like hemorrhoids or anal fissures, could indicate a more serious underlying issue that requires further investigation.
2.4 Personal and Family Medical History Individuals with a family history of colorectal cancer, polyps, or other gastrointestinal disorders should be particularly vigilant about rectal bleeding. If you have any pre-existing conditions like inflammatory bowel disease, it is important to monitor for any changes in symptoms and seek medical advice when necessary.
3. Diagnostic Approaches for Rectal Bleeding

3.1 Physical Examination The first step in diagnosing the cause of rectal bleeding often involves a physical examination by a healthcare provider. This may include an examination of the rectum and anus to check for visible signs of hemorrhoids, fissures, or other abnormalities.
3.2 Stool Tests Stool tests can help detect hidden blood in the stool (occult blood) or other markers that indicate a gastrointestinal issue. These tests may help identify conditions like colorectal cancer, infections, or ulcers.
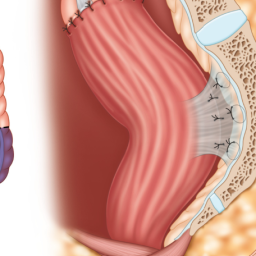
3.3 Endoscopy Procedures If the source of the bleeding is not immediately clear, your doctor may recommend an endoscopy to examine the inside of the gastrointestinal tract. Common procedures include:
- Colonoscopy: To examine the colon and rectum for polyps, cancer, or other conditions.
- Sigmoidoscopy: A similar procedure that examines the lower part of the colon and rectum.
- Upper Endoscopy (EGD): To look for bleeding from the stomach or upper gastrointestinal tract.
3.4 Imaging Tests In some cases, imaging tests such as CT scans or abdominal X-rays may be used to evaluate the extent of bleeding or to detect conditions like diverticulosis or tumors.
4. Treatment and Management of Rectal Bleeding
Treatment for rectal bleeding depends on the underlying cause. For example:
- Hemorrhoids: Can often be treated with over-the-counter creams, warm baths, and lifestyle changes.
- Anal Fissures: May be treated with topical ointments, increased fiber intake, and sitz baths.
- Colorectal Cancer: Requires surgical intervention, chemotherapy, or radiation, depending on the stage.
- Inflammatory Bowel Disease: Managed with medication to reduce inflammation and control symptoms.
- Diverticulosis: Managed with dietary changes, increased fiber intake, and sometimes antibiotics if diverticulitis occurs.
5. Prevention and Lifestyle Modifications
To prevent rectal bleeding, it is important to maintain a healthy lifestyle, including:
- Consuming a High-Fiber Diet to prevent constipation and reduce straining during bowel movements.
- Staying Hydrated to keep stools soft and promote healthy digestion.
- Regular Exercise to improve overall gastrointestinal health and prevent constipation.
- Avoiding Prolonged Sitting on the Toilet to reduce pressure on the rectum and anus.
Rectal bleeding, while common, can be caused by a range of conditions, from minor issues like hemorrhoids to more serious conditions like colorectal cancer. It is important to monitor symptoms and seek medical attention when necessary. Early diagnosis and intervention can help prevent complications and improve outcomes for those affected. Regular screening, a healthy diet, and lifestyle modifications can play a significant role in reducing the risk of rectal bleeding and its underlying causes.