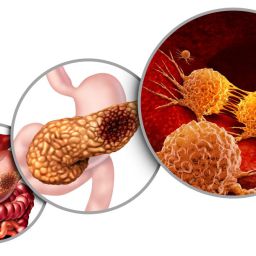
1. The Role of the Pancreas in Digestion
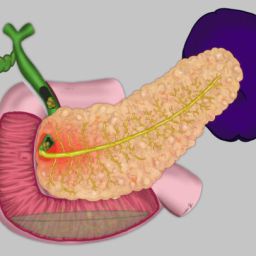
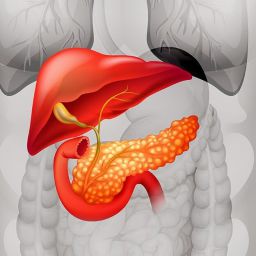
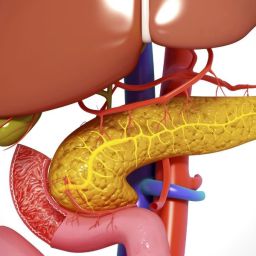
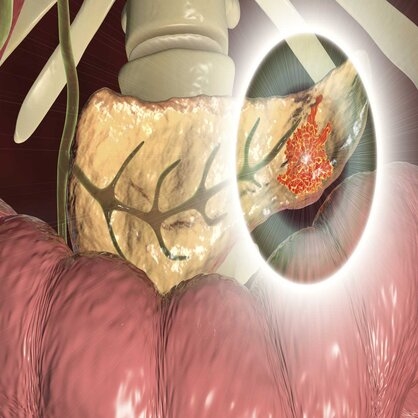
Before diving into the challenges and solutions, it is important to understand the pancreas’s role in the digestive process. The pancreas serves two major functions:
- Exocrine function: Producing digestive enzymes like amylase, lipase, and protease that break down carbohydrates, fats, and proteins in the small intestine.
- Endocrine function: Regulating blood sugar by secreting insulin and glucagon.
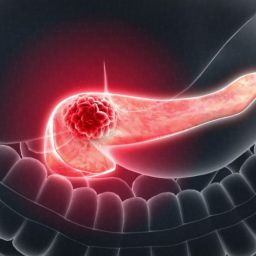
In patients with pancreatic cancer, the tumor may interfere with both functions, leading to difficulty in digesting food and managing blood sugar levels. Surgical removal of part or all of the pancreas, as well as chemotherapy and radiation, can further impair the pancreas’s ability to perform its roles, directly affecting nutrition.
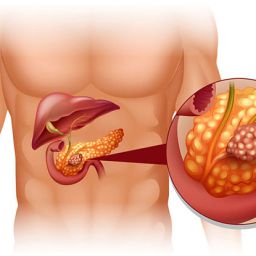
2. Nutritional Challenges in Pancreatic Cancer
2.1 Digestive Difficulties
As pancreatic cancer progresses, patients often experience symptoms such as nausea, bloating, and loss of appetite, which can make it difficult to eat enough to meet their energy and nutritional needs. Some of the specific digestive issues include:
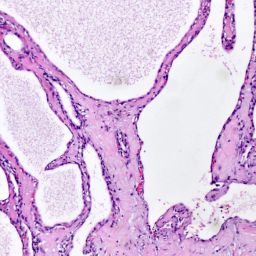
- Malabsorption: When the pancreas is unable to produce enough digestive enzymes, the body struggles to absorb fats and other nutrients. This can lead to weight loss, malnutrition, and fatigue.
- Steatorrhea (Fatty Stools): This condition occurs when undigested fat is excreted in the stool, leading to oily, foul-smelling stools. It is a sign of pancreatic insufficiency, where the pancreas cannot produce sufficient enzymes to break down fat.
- Early Satiety: Patients may feel full after eating only small amounts of food, leading to insufficient caloric intake.
2.2 Blood Sugar Imbalances
When the pancreas is compromised by cancer, patients may experience difficulties regulating blood sugar levels. This can manifest as:
- Hyperglycemia (High Blood Sugar): Insulin production may decrease, causing elevated blood glucose levels, especially after meals.
- Hypoglycemia (Low Blood Sugar): If insulin production fluctuates or is not well-regulated, patients may experience periods of low blood sugar, leading to dizziness, sweating, and fatigue.
Managing blood sugar levels becomes particularly challenging for patients with diabetes or pre-diabetes.
2.3 Taste Changes and Food Aversion
Pancreatic cancer treatment, including chemotherapy and radiation, can alter taste and smell, making previously enjoyable foods seem unappetizing or even repulsive. These changes may lead to:
- Taste Alterations: Chemotherapy can cause a metallic or bitter taste, making it hard to eat certain foods.
- Loss of Appetite: Chemotherapy-induced nausea, pain, or emotional distress can lead to a reduced desire to eat, which exacerbates the risk of malnutrition.
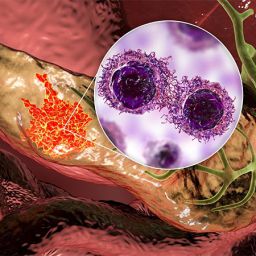
2.4 Weight Loss and Muscle Wasting
Patients with pancreatic cancer often experience significant weight loss, especially if the cancer affects the body’s ability to absorb nutrients. This is known as cachexia, a complex syndrome characterized by unintended weight loss, muscle wasting, and fatigue. Cachexia can affect a patient’s strength, immunity, and overall quality of life.
3. Nutritional Strategies for Pancreatic Cancer Patients
Given the numerous challenges associated with eating and digestion in pancreatic cancer, it is crucial to adopt a personalized nutrition plan that can help manage symptoms, maintain energy levels, and optimize health. Some strategies that can improve the nutritional status of pancreatic cancer patients include:

3.1 Enzyme Replacement Therapy (ERT)
For patients who experience pancreatic insufficiency, enzyme replacement therapy is a common treatment. These enzyme supplements, taken with meals, help improve digestion and nutrient absorption. Patients may need to take pancreatic enzymes for life, depending on the extent of their surgery or cancer.
- Digestive Enzymes: Pancreatic enzyme replacement products contain amylase, lipase, and protease to help the body break down carbohydrates, fats, and proteins.
3.2 Small, Frequent Meals
Eating small, frequent meals can help patients cope with early satiety and avoid overwhelming the digestive system. Instead of large meals, patients should aim to eat 5-6 small meals a day. Each meal should be well-balanced and high in calories to support energy needs.
- High-Calorie, Nutrient-Dense Foods: Since many patients have difficulty eating large amounts, it is important to include calorie-dense foods like nuts, seeds, avocados, and full-fat dairy products. Nutritional supplements such as protein shakes or smoothies can also help boost calorie intake.
3.3 Focusing on Protein Intake
Protein is crucial for healing, maintaining muscle mass, and immune function. Patients should aim to include adequate sources of protein in their meals, such as lean meats, fish, eggs, dairy, and plant-based proteins like beans and lentils.
- Protein Supplements: In cases of severe weight loss, protein shakes or powder supplements can help patients meet their protein needs without the need to eat large portions.
3.4 Managing Blood Sugar Levels
Patients who experience blood sugar imbalances should work closely with their healthcare team to monitor and regulate their glucose levels. A diet rich in fiber, lean protein, and healthy fats can help stabilize blood sugar.
- Low Glycemic Index Foods: Foods that have a low glycemic index (GI), such as whole grains, vegetables, and legumes, can help prevent spikes in blood sugar. Avoiding high-sugar and high-fat foods is essential.
3.5 Hydration and Electrolyte Balance
Staying hydrated is crucial for maintaining energy and preventing dehydration. Patients with pancreatic cancer may experience vomiting or diarrhea, which can lead to dehydration and electrolyte imbalances. Drinking fluids throughout the day and consuming electrolyte-rich drinks (e.g., coconut water or sports drinks) can help manage hydration.
3.6 Addressing Taste and Appetite Changes
To combat taste changes and loss of appetite, patients can try various strategies, such as:
- Adding flavor: Using herbs, spices, and marinades to make food more appealing.
- Cold foods: Cold or room temperature foods may be more palatable than hot meals, especially if taste alterations are present.
- Smaller portions with variety: Offering a variety of foods in small portions can help encourage eating despite reduced appetite.
3.7 Nutritional Supplements
Patients who cannot meet their nutritional needs through food alone may benefit from nutritional supplements. These supplements are specially formulated to provide essential vitamins, minerals, and calories. High-protein, high-calorie drinks or powders can be an important part of the diet to ensure adequate nutrition.
4. The Role of Dietitians and Healthcare Providers
Collaboration with a registered dietitian is essential in the management of nutrition for pancreatic cancer patients. A dietitian can:
- Develop a personalized nutrition plan that meets the patient’s specific needs, taking into account their medical history, type of surgery, and side effects of treatment.
- Provide advice on how to manage symptoms such as nausea, poor appetite, and digestive issues.
- Guide patients in making healthy food choices that support recovery, enhance quality of life, and help manage any co-existing conditions such as diabetes.
4.1 Psychological Support and Food Choices
In addition to medical and nutritional advice, patients may benefit from psychological support. Coping with the emotional and mental toll of cancer treatment can influence eating habits. Counseling or therapy can help patients manage stress, anxiety, and depression, which in turn can support healthier eating behaviors.
Nutrition plays a vital role in the treatment and recovery of pancreatic cancer patients. The impact of pancreatic cancer on digestion, absorption, and metabolism presents unique challenges, but with careful planning, the right interventions, and support from healthcare providers, many of these challenges can be managed. Proper nutrition can not only help prevent malnutrition and muscle wasting but also enhance recovery, manage side effects, and improve quality of life.
Patients are encouraged to collaborate with their healthcare team, including oncologists, dietitians, and other specialists, to develop a nutrition plan tailored to their specific needs. By prioritizing nutrition, patients with pancreatic cancer can better navigate their treatment journey and achieve the best possible outcomes.