1: Understanding Irritable Bowel Syndrome (IBS)
What is Irritable Bowel Syndrome (IBS)?
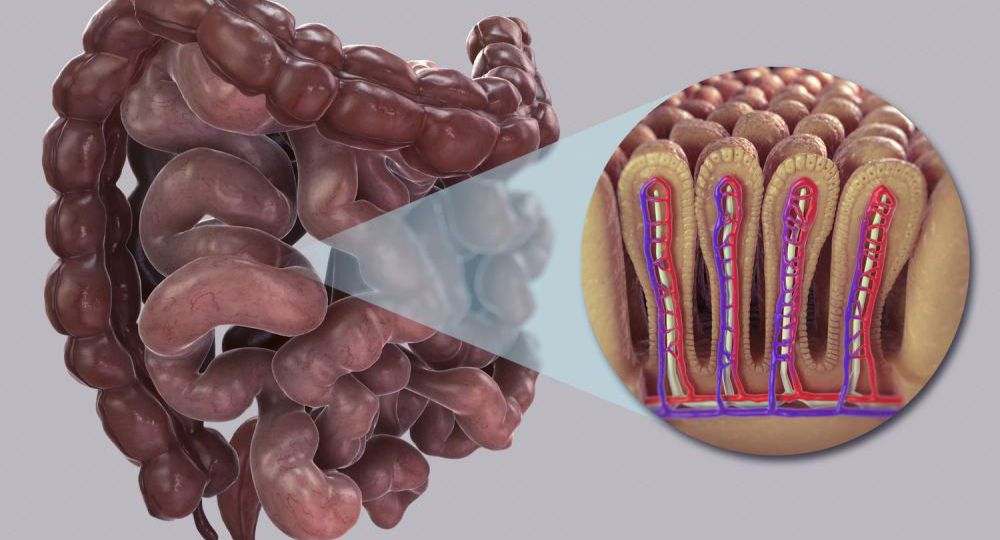
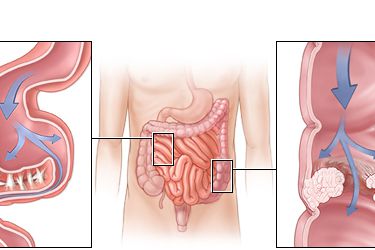
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder that affects the large and small intestines. Although it doesn’t cause visible damage to the intestines, it can disrupt the normal functioning of the digestive system. IBS is considered a syndrome because it encompasses a variety of symptoms, including:
- Abdominal pain and cramping
- Bloating and gas
- Diarrhea and/or constipation
- Altered bowel movements, such as mucus in the stool
- Nausea and fatigue
While IBS can affect anyone, it is more common in women and tends to develop before the age of 50. The exact cause of IBS is still uncertain, but factors such as gut-brain interactions, intestinal motility disturbances, food sensitivities, and increased stress levels are believed to play a role in triggering the symptoms.
Types of IBS
IBS can be categorized into different subtypes based on the predominant symptom:

- IBS-D (Diarrhea-predominant IBS): Characterized by frequent, urgent diarrhea and abdominal pain.
- IBS-C (Constipation-predominant IBS): Characterized by chronic constipation, infrequent bowel movements, and discomfort.
- IBS-M (Mixed IBS): Involves alternating episodes of diarrhea and constipation.
- IBS-U (Unsubtyped IBS): Symptoms do not consistently fit into the other categories.
While the underlying mechanism of IBS remains unknown, the symptoms can vary greatly between individuals, and triggers can differ based on diet, stress, and other factors.
2: Key Factors That Contribute to IBS
Understanding the key factors that contribute to IBS is essential for effective management. While the exact cause of IBS remains unknown, several contributing factors can influence the development and exacerbation of the disorder.
1. Gut Motility Issues
One of the main causes of IBS symptoms is the dysfunction of the muscles of the intestines, which affects the movement of food through the digestive tract. This can lead to either slow or rapid transit, contributing to constipation or diarrhea, respectively. These motility issues are often linked to abnormal signals between the brain and the gut.
2. Intestinal Sensitivity
People with IBS tend to have an increased sensitivity in the intestines, making them more prone to discomfort or pain when the digestive system is stimulated. This heightened sensitivity can result in bloating, cramping, and a feeling of fullness after eating.
3. Gut Microbiome Imbalance
Research suggests that an imbalance in the gut microbiome – the community of bacteria in the digestive tract – may play a role in the development of IBS. Disruptions in the normal balance of gut bacteria can contribute to symptoms like bloating, gas, and altered bowel movements.
4. Stress and Anxiety
Stress and emotional well-being are closely linked to gastrointestinal health. For many people with IBS, symptoms worsen during periods of high stress or anxiety. The gut-brain connection plays a significant role in the regulation of the digestive system, and psychological factors can influence gut motility and sensitivity.
3: Dietary Management of IBS
Dietary changes are often the first line of treatment for managing IBS. While there is no one-size-fits-all diet, many individuals find relief by making specific changes to their eating habits.
1. Low FODMAP Diet
The Low FODMAP Diet is one of the most effective dietary interventions for IBS. FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) are a group of short-chain carbohydrates that can be poorly absorbed in the small intestine, leading to fermentation in the gut and causing symptoms like gas, bloating, and diarrhea.
The Low FODMAP diet involves eliminating high-FODMAP foods for a period of time and then gradually reintroducing them to identify which ones trigger symptoms. Common high-FODMAP foods to avoid include:
- Dairy products (milk, yogurt)
- Certain fruits (apples, pears, watermelon)
- Certain vegetables (onions, garlic, cauliflower)
- Legumes and beans
2. Fiber Management
Fiber plays an important role in digestion, and managing fiber intake can help control symptoms. For those with IBS-C (constipation-predominant IBS), increasing fiber intake, especially soluble fiber, can help improve bowel movements. Foods like oats, psyllium, and chia seeds are good sources of soluble fiber.
For those with IBS-D (diarrhea-predominant IBS), too much insoluble fiber can worsen symptoms, so reducing foods like whole wheat and raw vegetables might be helpful.
3. Probiotics and Gut Health
Probiotics are beneficial bacteria that can help restore balance to the gut microbiome, which may be disrupted in individuals with IBS. Some studies suggest that specific strains of probiotics can help reduce bloating, gas, and other IBS symptoms. Fermented foods like yogurt, kefir, and sauerkraut are natural sources of probiotics, but supplements can also be considered for targeted relief.
4: Medications for IBS Management
While dietary changes are fundamental, medications may be necessary for some individuals to manage more severe symptoms of IBS. Medications are typically used when lifestyle and dietary interventions are not enough to provide relief.
1. Antispasmodic Medications
For individuals who experience cramping and abdominal pain, antispasmodic medications can help relax the muscles of the intestines. These medications can reduce pain and discomfort by alleviating muscle spasms in the digestive tract.
2. Laxatives
For individuals with IBS-C (constipation-predominant IBS), mild laxatives may be recommended to ease bowel movements. However, long-term use of laxatives should be monitored, as they can lead to dependency.
5: Lifestyle Changes for IBS Management
Beyond dietary changes and medications, lifestyle modifications can also play a key role in managing IBS.
1. Stress Management
Since stress is a major trigger for many IBS sufferers, finding effective ways to manage stress is critical for symptom relief. Practices such as:
- Mindfulness meditation
- Deep breathing exercises
- Yoga and tai chi
- Cognitive-behavioral therapy (CBT)
can all help reduce stress and anxiety, improving gut function and overall well-being.
2. Regular Exercise
Exercise is beneficial for digestion and overall health. For individuals with IBS, regular physical activity can help improve bowel regularity, reduce stress, and promote a sense of well-being. Activities like walking, swimming, and cycling are gentle on the body and beneficial for gut health.
3. Sleep Hygiene
Good sleep is essential for overall health, and poor sleep can worsen IBS symptoms. Ensuring adequate and quality sleep can improve the body’s ability to cope with stress and support digestion. Establishing a consistent sleep schedule, limiting caffeine, and practicing relaxation techniques before bed can all improve sleep quality.
Managing small intestine inflammation (IBS) requires a multifaceted approach that includes dietary changes, medication, stress management, and lifestyle adjustments. While IBS is a chronic condition, it is possible to manage symptoms effectively and improve quality of life with the right combination of treatments.
Each individual with IBS is unique, and what works for one person may not work for another. Therefore, it is essential for IBS patients to work closely with healthcare professionals, including gastroenterologists, dietitians, and mental health experts, to develop a personalized treatment plan that addresses their specific needs.
By understanding the factors that contribute to IBS and taking a proactive approach to managing symptoms, individuals can lead a healthy, active life with minimal disruption from their digestive issues.



