1. Understanding Liver Adenomas
Liver adenomas are benign, non-cancerous growths in the liver, primarily made up of hepatocytes, the cells responsible for liver function. These tumors are often found in individuals between the ages of 20 and 40, with a higher prevalence in women, especially those who have taken oral contraceptives or hormone replacement therapy. While most liver adenomas do not cause symptoms, their potential for complications such as hemorrhage, rupture, or malignant transformation makes them a concern in certain cases.
1.1 Causes and Risk Factors of Liver Adenomas
The exact cause of liver adenomas is not entirely understood, but several factors contribute to their development:

- Hormonal Influence: One of the most significant risk factors for liver adenomas is the use of oral contraceptives or hormone replacement therapy, both of which increase estrogen levels. Estrogen is thought to promote the growth of these tumors, making women more susceptible to developing them.
- Genetic Factors: Some genetic conditions, such as familial adenomatous polyposis (FAP) and glycogen storage disease, can predispose individuals to liver adenomas. These inherited disorders can lead to an increased number of adenomas or even malignant transformation.
- Obesity and Diabetes: There is growing evidence that metabolic conditions like obesity and diabetes may contribute to the development of liver adenomas. Excessive fat accumulation in the liver (non-alcoholic fatty liver disease) may promote tumor growth.
- Alcohol Consumption: While liver adenomas are not directly linked to alcohol consumption, chronic liver disease caused by excessive alcohol intake may increase the risk of developing liver tumors.
2. Are Liver Adenomas Dangerous?
While liver adenomas are generally benign, certain complications can arise that make them dangerous. These complications include hemorrhage, rupture, and the potential for malignant transformation. Below are the key risks associated with liver adenomas:
2.1 Risk of Bleeding
One of the most significant dangers of liver adenomas is the risk of bleeding. Adenomas are vascular lesions, meaning they contain blood vessels that can be prone to rupture, leading to internal bleeding. In some cases, this bleeding may be spontaneous and severe enough to cause shock. Patients with larger adenomas or those that have been present for a longer period are at a higher risk of bleeding.
The risk of hemorrhage increases with the size of the adenoma, with tumors larger than 5 cm being particularly susceptible to rupture. Women who use oral contraceptives are also at a higher risk of bleeding, as hormonal factors may make the blood vessels in adenomas more fragile.
2.2 Rupture and Life-Threatening Complications
In addition to bleeding, liver adenomas may rupture, which can lead to severe abdominal pain, shock, and even life-threatening complications. Rupture typically occurs in larger adenomas, and the risk increases with pregnancy, due to the hormonal changes that occur during this period. Although rare, a ruptured liver adenoma is a medical emergency requiring immediate treatment.
2.3 Malignant Transformation
Though rare, there is a potential for liver adenomas to transform into a form of liver cancer, such as hepatocellular carcinoma (HCC). The risk of malignant transformation is particularly high in patients with large adenomas, those with a history of chronic liver disease, and those with certain genetic predispositions. The transformation of a liver adenoma into a malignant tumor is more likely in patients with Glycogen Storage Disease Type 1, which is linked to multiple adenomas.
Malignant transformation is one of the primary reasons why liver adenomas require careful monitoring, especially if they exhibit growth or atypical characteristics.
3. How Are Liver Adenomas Diagnosed?
Liver adenomas are often diagnosed incidentally during imaging studies conducted for other conditions. However, when symptoms such as abdominal pain, nausea, or vomiting arise, a thorough diagnostic process is necessary. The following diagnostic methods are used to detect and assess liver adenomas:
3.1 Imaging Studies
- Ultrasound: This is usually the first imaging technique used to detect liver adenomas. It is non-invasive, affordable, and effective in identifying liver masses. However, ultrasound may not always provide enough detail to differentiate adenomas from other liver lesions.
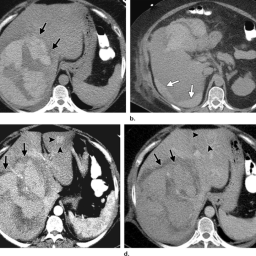
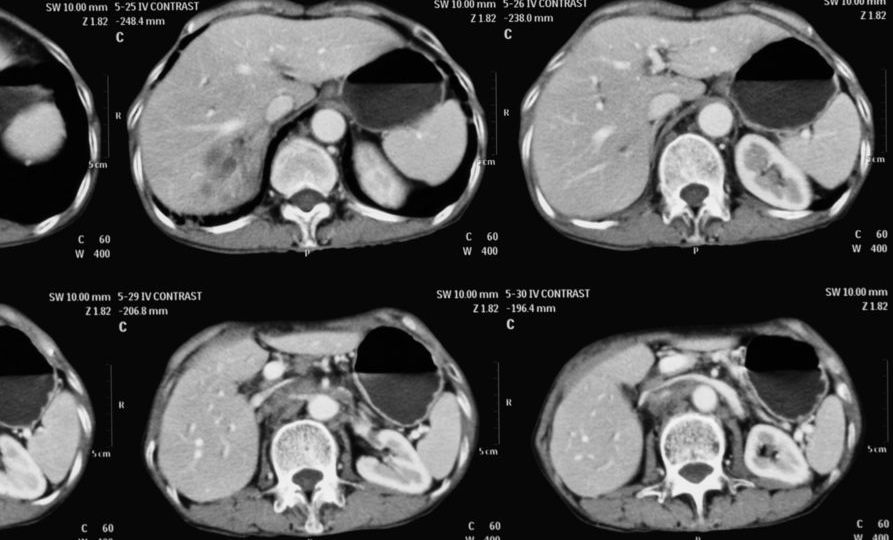
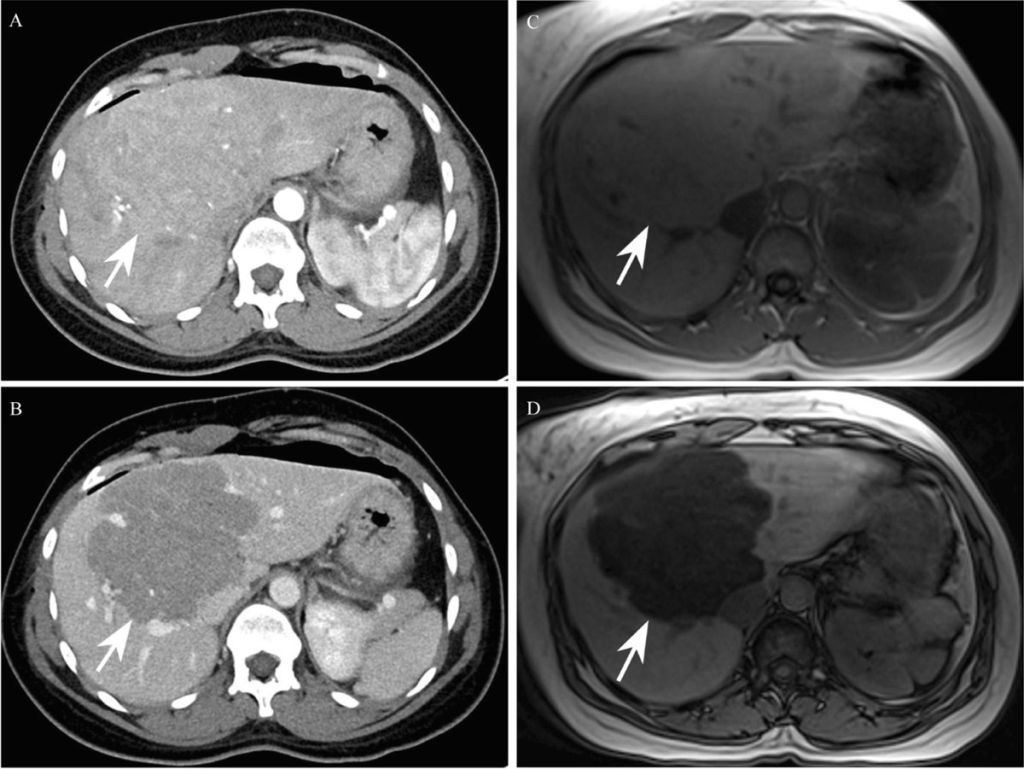
- CT Scan: A contrast-enhanced computed tomography (CT) scan provides more detailed images of the liver, helping doctors better understand the size, location, and vascularity of the adenomas. This imaging is often used to monitor the growth of existing adenomas and detect complications such as hemorrhage.
- MRI: Magnetic resonance imaging (MRI) is considered the gold standard for diagnosing liver adenomas. MRI can provide high-resolution images of the liver and identify characteristic features of adenomas, such as their size, structure, and blood vessel involvement. MRI is particularly useful in assessing the risk of complications like rupture and bleeding.
3.2 Biopsy
While imaging is typically sufficient for diagnosis, in some cases, a liver biopsy may be performed to confirm the benign nature of the adenoma or to rule out malignancy. A biopsy involves taking a small sample of tissue from the adenoma for laboratory analysis. This procedure is typically reserved for cases where the imaging results are inconclusive or where there is a concern about malignant transformation.
4. When Is Surgery Necessary for Liver Adenomas?
Although many liver adenomas do not require surgery and can be safely monitored, there are certain circumstances in which surgical intervention becomes necessary. The decision to undergo surgery is based on factors such as the size of the adenoma, the risk of complications, and whether the tumor exhibits atypical features.
4.1 Size of the Adenoma
Surgical removal of liver adenomas is often recommended when the tumor exceeds a certain size, typically 5 cm or larger. Larger adenomas have a higher risk of hemorrhage, rupture, and malignant transformation, making surgery a more attractive option. Adenomas larger than 10 cm are particularly concerning and are more likely to cause significant complications.
4.2 Symptomatic Adenomas
If a liver adenoma causes symptoms, such as pain or discomfort, surgery may be considered to relieve these symptoms. Adenomas that cause significant pain, bleeding, or liver dysfunction may require removal to prevent further complications and improve the patient’s quality of life.
4.3 Risk of Malignant Transformation
In patients with liver adenomas that show signs of malignant transformation, surgical removal is essential to prevent the spread of cancer. The presence of characteristics such as rapid growth, irregular borders, or atypical features on imaging studies may prompt the need for surgical intervention to obtain a tissue sample and perform a more definitive diagnosis.
4.4 Pregnancy
Pregnant women with large liver adenomas are at an increased risk of complications, including rupture and bleeding. If a liver adenoma is diagnosed during pregnancy and is causing significant problems, surgical intervention may be required. However, the timing of surgery should be carefully considered, as surgery during pregnancy carries risks to both the mother and the fetus.
4.5 Non-Response to Medical Management
In cases where liver adenomas do not respond to medical management, including the cessation of oral contraceptives or hormone therapy, and continue to grow or cause complications, surgery may be necessary. Surgery may involve either laparoscopic or open resection of the adenoma, depending on its location and size.
5. Surgical Options for Liver Adenomas
Surgical options for liver adenomas typically include:
5.1 Laparoscopic Resection
Laparoscopic resection is a minimally invasive procedure that involves the removal of the adenoma through small incisions. This method offers quicker recovery times, less postoperative pain, and a lower risk of infection compared to traditional open surgery.
5.2 Open Resection
In some cases, open resection may be required, especially for larger adenomas or those located in difficult-to-reach areas of the liver. This procedure involves making a larger incision in the abdomen to access the liver and remove the adenoma.
5.3 Liver Transplantation
In rare cases, when the liver adenomas are recurrent or multiple and are associated with underlying liver disease (such as glycogen storage disease), a liver transplant may be considered.
Liver adenomas are generally benign tumors that do not pose an immediate threat. However, they can lead to serious complications such as bleeding, rupture, or malignant transformation in certain circumstances. Surgical intervention is typically required when the adenoma is large, symptomatic, or shows signs of malignancy. Early detection through imaging, along with careful monitoring, is crucial for managing the condition and preventing complications. For patients with liver adenomas, personalized treatment strategies based on size, symptoms, and risk factors are essential in optimizing outcomes and ensuring long-term health.