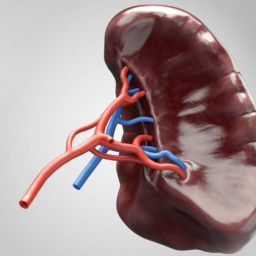
1. Conditions Requiring Splenectomy
There are several reasons why a splenectomy may be required. Below are some of the most common medical conditions that necessitate the removal of the spleen:
a. Trauma and Injury to the Spleen
One of the most common reasons for splenectomy is trauma or injury to the spleen. In cases of blunt trauma, such as car accidents or sports injuries, the spleen can be ruptured or severely damaged. When the injury causes significant bleeding or is life-threatening, the removal of the spleen may be the only viable option to save the patient’s life. In some cases, less invasive methods like embolization may be used to control bleeding, but if these fail, splenectomy becomes essential.
b. Blood Disorders
Certain blood disorders may also lead to the need for splenectomy. For example:

- Idiopathic Thrombocytopenic Purpura (ITP): In ITP, the body’s immune system mistakenly destroys platelets, leading to a low platelet count and increased risk of bleeding. Splenectomy is often considered when other treatments fail to stabilize platelet counts.
- Hereditary Spherocytosis: This is a genetic condition where red blood cells are abnormally shaped, making them more prone to destruction in the spleen. Splenectomy can help prevent the breakdown of red blood cells, improving the patient’s symptoms.
- Sickle Cell Disease: In patients with sickle cell disease, the spleen often becomes enlarged and functions poorly, leading to complications. In some cases, splenectomy can be performed to reduce the risk of infections and improve blood circulation.
- Thalassemia: In thalassemia, a blood disorder characterized by abnormal hemoglobin production, the spleen can become enlarged due to the excessive destruction of abnormal red blood cells. Splenectomy may be needed to relieve symptoms of splenomegaly and improve blood health.
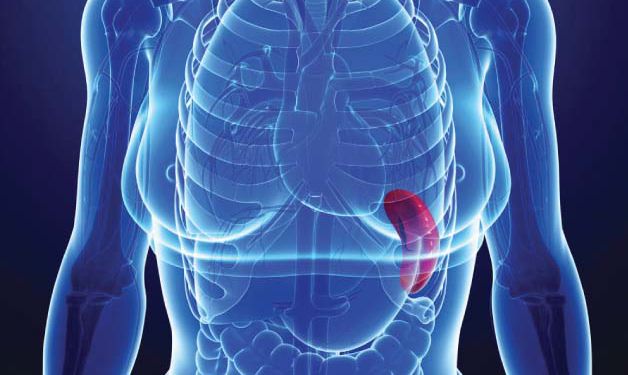
c. Splenomegaly
Splenomegaly refers to an enlarged spleen, which can occur due to various conditions such as liver disease, certain cancers, or infections. When the spleen becomes abnormally large, it can cause pain, discomfort, and other complications. If conservative treatments fail, splenectomy may be considered.
d. Cancers Involving the Spleen
Certain types of cancers, including lymphoma, leukemia, and splenic tumors, may affect the spleen. In cases where the spleen is involved in cancer or is at risk of metastasis, splenectomy might be necessary to prevent the spread of cancer or to alleviate symptoms related to splenic involvement.
e. Infections
Though rare, the spleen can become infected by bacterial or parasitic organisms, leading to serious health risks. In certain cases, an infection may cause the spleen to become abscessed or severely damaged. If antibiotics and other treatments are ineffective, splenectomy may be required to prevent the spread of infection.
f. Autoimmune Diseases
Some autoimmune diseases, such as systemic lupus erythematosus (SLE), can lead to the spleen becoming enlarged or dysfunctional. In these conditions, the immune system attacks the spleen, leading to inflammation and potentially impairing its function. In some instances, removing the spleen can help alleviate symptoms and improve the patient’s quality of life.
2. Benefits of Splenectomy
While the spleen plays a significant role in immune defense and blood filtration, its removal can still offer several benefits, particularly when it is necessary for the treatment of certain conditions. Here are the key advantages of splenectomy:

a. Relief from Pain and Discomfort
In cases of splenomegaly or blood disorders, the spleen can become enlarged and cause significant discomfort. Removing the spleen can provide immediate relief from the pain and bloating associated with these conditions. Patients who suffer from an enlarged spleen often report feeling more comfortable after the procedure.
b. Improved Blood Counts
In conditions such as ITP or hereditary spherocytosis, where the spleen destroys platelets or red blood cells prematurely, splenectomy can lead to an improvement in blood counts. For patients with low platelet counts, the removal of the spleen may help stabilize the condition, reducing the need for medications or blood transfusions.
c. Prevention of Life-Threatening Complications
For patients with certain blood disorders, such as sickle cell disease, the spleen can become a source of frequent infections and complications. Splenectomy can help prevent these issues by removing an organ that is functioning abnormally. Additionally, in cases of trauma or cancer, splenectomy can save the patient’s life by removing damaged tissue or cancerous growths.
d. Treatment of Refractory Conditions
For some patients, splenectomy is considered a last-resort treatment when other therapies fail. Conditions like chronic idiopathic thrombocytopenic purpura (ITP) or autoimmune disorders can be resistant to drug treatments, and removing the spleen may be the only option for improving symptoms and quality of life.
e. Improved Immune Function (in some cases)
In some patients, particularly those with enlarged spleens or splenic dysfunction, splenectomy can help restore more normal immune function. Although the spleen plays a vital role in the immune system, removing it may sometimes improve overall health, particularly if the spleen is malfunctioning or overloaded with damaged cells.
3. Risks and Considerations of Splenectomy
While splenectomy can offer significant benefits, it is not without risks. Patients who undergo splenectomy are at a higher risk for certain complications:
a. Increased Risk of Infections
The spleen plays a key role in filtering out bacteria from the blood and fighting infections. After splenectomy, the body’s ability to defend against certain infections, particularly bacterial infections, may be compromised. As a result, patients who have had their spleens removed are often advised to receive vaccinations and prophylactic antibiotics to reduce their risk of infection, especially against pneumococcus, meningococcus, and Haemophilus influenzae.
b. Post-Splenectomy Sepsis
Post-splenectomy sepsis (PSS) is a potentially life-threatening condition that can occur due to infections after splenectomy. Patients who have undergone the procedure must be vigilant in seeking medical attention if they experience signs of infection, such as fever or chills, and should take measures to prevent infection.
c. Long-Term Health Monitoring
Patients who have had their spleen removed must be monitored for long-term health concerns. Regular check-ups, including blood tests, are necessary to ensure that no complications, such as an increased risk of blood clots or other infections, develop over time.
Splenectomy is a critical procedure in the treatment of several medical conditions, particularly when the spleen becomes diseased, damaged, or dysfunctional. Although the procedure is not without risks, the benefits of splenectomy—such as pain relief, improved blood counts, and prevention of life-threatening complications—can be life-changing for many patients. With proper post-operative care, including vaccinations and careful monitoring, individuals who undergo splenectomy can lead healthy lives, with a reduced risk of infections and a better quality of life.
In conclusion, splenectomy remains an essential surgical option for managing various blood disorders, trauma, and infections, offering hope and healing to those who require it.