What Causes an Inguinal Hernia?
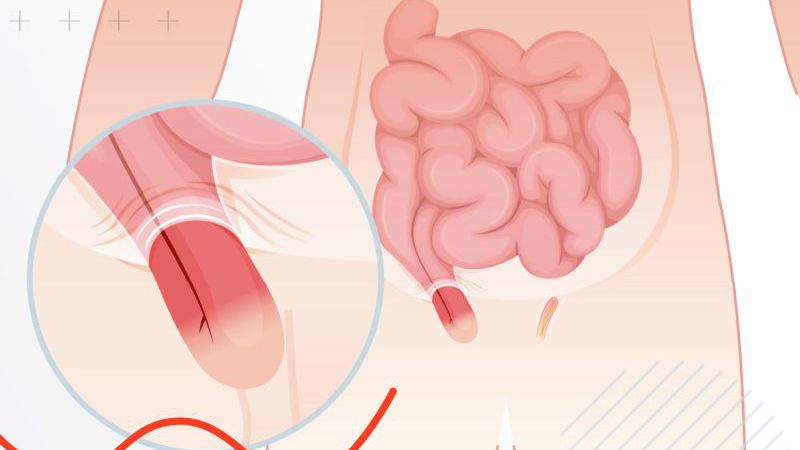
The most common causes of inguinal hernias are increased pressure within the abdomen, congenital weakness in the abdominal wall, and muscle strain. Several factors contribute to the development of an inguinal hernia, including:
- Straining: Chronic coughing, heavy lifting, or straining during bowel movements can lead to increased pressure in the abdominal cavity, which may push tissue through a weak spot.
- Age and Gender: Men are more prone to inguinal hernias due to their anatomy. Additionally, older individuals may experience weakened abdominal muscles, making hernias more likely.
- Obesity: Excess weight places added pressure on the abdominal wall, increasing the risk of developing a hernia.
- Previous Surgery: Individuals who have had previous hernia repairs may be at risk for developing another hernia, particularly if the area has weakened over time.
What Causes Back Pain?
Back pain is one of the most common medical complaints globally. It can range from mild discomfort to severe, debilitating pain that interferes with daily activities. The causes of back pain are numerous and often involve complex interactions between the bones, muscles, ligaments, and nerves that make up the spine.
Some common causes of back pain include:
- Muscle Strain: Lifting heavy objects or sudden movements can cause muscle strain, leading to pain and discomfort in the lower back.
- Herniated Discs: When the discs between the vertebrae in the spine bulge or rupture, they can put pressure on nearby nerves, causing back pain.
- Degenerative Conditions: Conditions such as osteoarthritis or degenerative disc disease can lead to wear and tear on the spine, resulting in chronic back pain.
- Postural Issues: Poor posture, especially when sitting for long periods, can lead to musculoskeletal imbalances that contribute to back pain.
- Injury or Trauma: Accidents, falls, or other forms of physical trauma can cause damage to the spine, muscles, or nerves, resulting in pain.
The Relationship Between Inguinal Hernia and Back Pain
While an inguinal hernia and back pain may seem like two distinct health issues, there are several ways in which they can be related. The relationship between these conditions can be explained through both anatomical and functional connections.
1. Postural Changes Due to Hernia Pain
One of the most common ways in which inguinal hernias and back pain are connected is through postural changes. When a person experiences pain or discomfort from an inguinal hernia, they may alter their posture to relieve pressure or avoid aggravating the hernia. These compensatory movements can lead to imbalances in the spine, resulting in strain on the lower back muscles and potentially leading to back pain.
- Imbalanced Gait: People with an inguinal hernia may adjust their walking pattern to avoid discomfort in the groin area. This change in gait can affect the alignment of the spine, contributing to muscle tension and back pain.
- Pelvic Tilt: Chronic pain from an inguinal hernia may cause individuals to unconsciously tilt their pelvis forward or backward to alleviate pressure in the groin. This misalignment can strain the lower back muscles, leading to pain.
2. Increased Abdominal Pressure
As mentioned earlier, one of the main causes of inguinal hernias is increased abdominal pressure. Similarly, increased abdominal pressure can also affect the spine, particularly the lower back. The abdomen and lower back are interconnected through the core muscles, and any change in intra-abdominal pressure can have an impact on spinal health.
- Increased Pressure on the Spine: When the abdominal wall is weakened due to a hernia, it can cause an imbalance in pressure distribution throughout the torso. This can place additional strain on the muscles and ligaments supporting the spine, contributing to back pain.
- Core Weakness: The muscles of the abdomen and lower back work together to stabilize the body. A hernia can weaken the abdominal muscles, which in turn can affect the strength and stability of the lower back muscles, leading to pain and discomfort.
3. Nerve Irritation and Compression
Another mechanism by which inguinal hernias can contribute to back pain is through nerve irritation. Inguinal hernias can sometimes irritate or compress nearby nerves, particularly in the pelvic and lower abdominal regions. These nerves can refer pain to the lower back, leading to symptoms that mimic typical back pain.
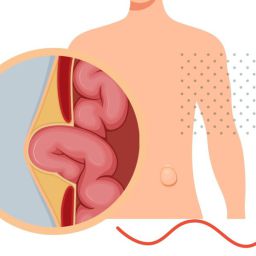
- Nerve Entrapment: When the hernia protrudes through the abdominal wall, it can compress surrounding tissues and nerves. This compression can lead to radiating pain in the lower back and legs, similar to sciatica.
- Referred Pain: The nerves in the lower abdomen and pelvis share pathways with those in the lower back. Therefore, pain originating from an inguinal hernia may be felt in the back as referred pain.
4. Chronic Strain from Hernia Complications
In some cases, untreated or poorly managed inguinal hernias can lead to complications that exacerbate back pain. For example, if the hernia becomes incarcerated or strangulated (when the blood supply to the herniated tissue is cut off), it can lead to severe pain in the groin area. This intense pain may cause individuals to adopt positions that increase strain on the back, leading to chronic back pain.
- Muscle Overuse: In an effort to avoid hernia pain, individuals may overuse certain muscle groups to compensate for the discomfort. This can lead to muscle fatigue and back pain, especially if the body is consistently in an abnormal posture.
Managing Both Conditions: Treatment and Relief
When both inguinal hernia and back pain are present, treatment becomes more complex, as addressing one condition may inadvertently affect the other. However, with appropriate care, both conditions can be managed effectively.
1. Inguinal Hernia Treatment
The treatment for an inguinal hernia typically involves surgical intervention. Depending on the severity of the hernia and the associated symptoms, surgery may be recommended to repair the hernia and prevent complications.
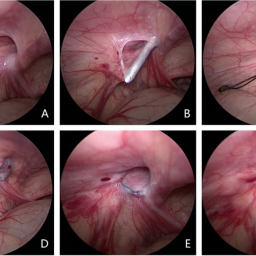
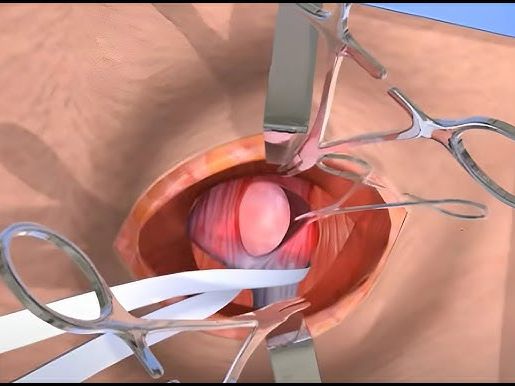
- Open Surgery: Involves making an incision in the groin area to push the herniated tissue back into place and reinforce the abdominal wall with mesh.
- Laparoscopic Surgery: A minimally invasive approach that uses small incisions and a camera to guide the surgeon in repairing the hernia.
If surgery is not immediately required, conservative treatments such as wearing a truss or abdominal binder may provide temporary relief.
2. Back Pain Management
Back pain management often involves a combination of physical therapy, lifestyle adjustments, and pain management techniques. Some common treatment options include:
- Physical Therapy: Targeted exercises to strengthen the back and core muscles can help alleviate pain and improve posture.
- Pain Relief Medications: Over-the-counter pain medications, such as ibuprofen or acetaminophen, may help manage mild to moderate back pain.
- Postural Training: Learning proper posture and ergonomics can reduce strain on the lower back and prevent further pain.
- Heat and Cold Therapy: Applying heat or cold packs can provide temporary relief from back pain by reducing inflammation and soothing muscle tension.
3. Addressing Both Conditions Simultaneously
For individuals suffering from both inguinal hernia and back pain, it is crucial to treat both conditions simultaneously. This may involve:
- Coordinated Care: Working with both a surgeon for the hernia and a physical therapist or chiropractor for the back pain.
- Lifestyle Adjustments: Making lifestyle changes, such as avoiding heavy lifting, maintaining a healthy weight, and engaging in low-impact exercise, can help prevent exacerbating either condition.
The relationship between inguinal hernia and back pain is complex but often intertwined. While the two conditions may seem separate, they share common risk factors, such as increased abdominal pressure, muscle strain, and postural changes, which can link them together. Addressing both conditions through proper diagnosis, treatment, and lifestyle changes can help individuals find relief and improve their overall quality of life. If you experience both inguinal hernia and back pain, seeking medical advice is essential to develop a comprehensive treatment plan tailored to your needs.