GIST
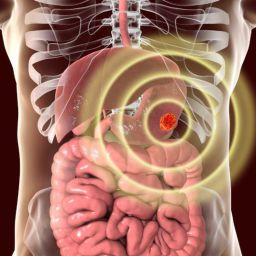
GISTs can develop anywhere along the gastrointestinal (GI) tract, with the stomach being the most common site. They can also occur in the small intestine, colon, rectum, and esophagus, although less frequently. These tumors are thought to originate from the interstitial cells of Cajal (ICCs), which are part of the GI tract’s nervous system and play a role in regulating motility.
Unlike other cancers, GISTs don’t often present with the usual symptoms of cancer such as weight loss or fever, making them difficult to detect in their early stages. However, as they grow, they may cause pain, bleeding, and changes in bowel movements. Diagnosis generally involves a combination of clinical evaluation, imaging studies, biopsy, and molecular testing.
In this article, we will explore the steps involved in diagnosing GIST and the various tests used to confirm the presence of the tumor.
2. Clinical Evaluation and Symptoms
The first step in diagnosing GIST usually involves a clinical evaluation by a physician. The patient’s medical history, symptoms, and a physical exam are key components of this evaluation. However, many symptoms of GIST are nonspecific and can be mistaken for other GI disorders.
Some common symptoms that may lead to a GIST diagnosis include
- Abdominal pain or discomfort: This is one of the most common symptoms. As GISTs grow, they can cause pain due to pressure on surrounding organs or tissues.
- Gastrointestinal bleeding: Blood in the stool or vomit can occur if the tumor ulcerates and bleeds.
- Bloating or a mass in the abdomen: A palpable mass may be felt during physical examination in some cases.
- Difficulty swallowing (in cases of tumors in the esophagus): This can occur if the tumor obstructs the digestive tract.
- Unexplained weight loss or nausea: These symptoms are more likely in advanced cases or when the tumor causes complications.
Since GIST symptoms often mimic those of other gastrointestinal conditions (e.g., ulcers, diverticulitis, Crohn’s disease), the physician will likely proceed with more specific diagnostic tests.
3. Imaging Tests
Imaging tests play a critical role in detecting GISTs and assessing their size, location, and spread. Several different imaging modalities are used to visualize the tumor and determine its characteristics.
3.1. CT Scan (Computed Tomography)
A CT scan is one of the most common imaging techniques used to diagnose GISTs. It provides detailed cross-sectional images of the body, allowing doctors to detect abnormal growths within the abdominal or pelvic region. CT scans are particularly useful for identifying the size and location of the tumor, as well as any spread to nearby organs or lymph nodes.
- Advantages: CT scans can detect GISTs even when they are small and asymptomatic. They are also essential for staging the tumor (determining how far it has spread).
- Limitations: A CT scan can only detect structural abnormalities and does not provide information on the tumor’s cellular characteristics.
3.2. MRI (Magnetic Resonance Imaging)
MRI is another imaging technique used to evaluate GISTs, especially for tumors located in the liver or pelvis, which may not be as easily accessible via CT. MRI uses magnetic fields and radio waves to produce detailed images of the internal organs.
- Advantages: MRI offers high-resolution images of soft tissues, making it particularly helpful in assessing GISTs located near or in contact with other soft tissues, such as blood vessels.
- Limitations: MRI is more expensive and less widely available compared to CT, and it may take longer to conduct.
3.3. Endoscopy and Endoscopic Ultrasound
In cases where a GIST is suspected to be located in the stomach or small intestine, endoscopy may be performed. An endoscope (a long, flexible tube with a camera) is inserted through the mouth or anus to visually examine the GI tract. If a tumor is found, an endoscopic ultrasound (EUS) may be used to evaluate its size and depth of penetration into the wall of the GI tract.
- Advantages: EUS can provide valuable information about the tumor’s size, location, and involvement with surrounding tissues. It also allows for tissue biopsy.
- Limitations: Endoscopy is not as useful for detecting GISTs located in the large intestine or areas that are harder to reach.
3.4. PET Scan (Positron Emission Tomography)

A PET scan can be used to detect metastasis (spread) of the tumor. It involves injecting a small amount of radioactive glucose into the body. Tumor cells tend to absorb more glucose than normal cells, allowing the scan to highlight areas of abnormal activity.
- Advantages: PET scans can detect cancer spread, even at an early stage.
- Limitations: PET scans are generally used in conjunction with other imaging studies and are not usually the first line of testing.
4. Biopsy
A biopsy involves the removal of a small sample of tissue from the suspected tumor for examination under a microscope. This is the most definitive way to diagnose GIST, as it allows pathologists to examine the cells for characteristics indicative of the tumor.
4.1. Needle Biopsy
In a needle biopsy, a thin needle is inserted into the tumor (guided by imaging techniques like CT or ultrasound) to collect tissue samples. The tissue is then analyzed for cancerous cells.
- Advantages: This method is minimally invasive and provides a quick sample for diagnosis.
- Limitations: Needle biopsy may not provide enough tissue for a conclusive diagnosis if the tumor is located in an area that is hard to access.
4.2. Surgical Biopsy
If a needle biopsy is not feasible, or if larger tissue samples are needed, a surgical biopsy may be performed. In this procedure, part or all of the tumor is surgically removed for analysis.
- Advantages: Provides a larger sample of tissue, which may improve diagnostic accuracy.
- Limitations: More invasive than a needle biopsy and carries greater risk.
5. Molecular Testing
One of the hallmarks of GISTs is their mutation in certain genes. The most common mutation occurs in the KIT gene (about 70-80% of GISTs) or the PDGFRA gene (about 5-10% of GISTs). Molecular testing of the tumor’s genetic material is crucial for confirming the diagnosis of GIST and for determining the appropriate treatment plan.
5.1. Immunohistochemistry (IHC)
Immunohistochemistry is a laboratory technique used to detect the presence of specific proteins in the tumor tissue. In GIST, IHC testing is typically done to check for the overexpression of the KIT protein, which is commonly found in GIST cells.
- Advantages: IHC helps in confirming whether a tumor is a GIST by detecting the characteristic KIT or PDGFRA proteins.
- Limitations: While IHC is a valuable diagnostic tool, it may not provide definitive answers in all cases, especially when the tumor lacks typical genetic mutations.
5.2. Molecular Genetic Testing (PCR or Sequencing)
Polymerase chain reaction (PCR) and sequencing tests can identify specific mutations in the KIT or PDGFRA genes. These tests are especially useful in cases where IHC results are inconclusive or when there is a need to assess the tumor’s risk for recurrence.
- Advantages: Genetic testing provides a more precise diagnosis and can guide treatment decisions, particularly with targeted therapies.
- Limitations: Genetic testing requires specialized labs and can be time-consuming.
6. Genetic Counseling and Risk Assessment
Genetic counseling may be recommended for patients diagnosed with GIST, particularly if there is a family history of GISTs or other genetic conditions. A genetic counselor can provide information on inherited mutations, risk of recurrence, and the implications for family members. Genetic testing of relatives may also be recommended if there is a hereditary form of GIST.
7. Staging of GIST
Once a diagnosis of GIST is confirmed, staging is necessary to determine the extent of the disease. Staging typically involves assessing the tumor’s size, its growth into surrounding tissues, and whether it has spread to distant organs or lymph nodes. Staging can help guide treatment choices and provide an outlook on prognosis.
The most widely used staging system for GIST is the American Joint Committee on Cancer (AJCC) system, which is based on:
- Tumor size
- The degree of spread to nearby lymph nodes or organs
- Whether the tumor is localized or metastatic
Diagnosing GIST is a complex process that involves a combination of clinical evaluation, imaging studies, biopsy, and molecular testing. Early and accurate diagnosis is key to effective treatment, as GISTs can behave differently depending on their size, location, and genetic makeup. By using a variety of diagnostic tools, healthcare providers can obtain a comprehensive understanding of the tumor, ultimately helping to guide treatment decisions and improve patient outcomes.