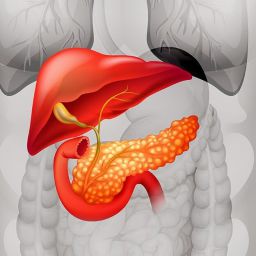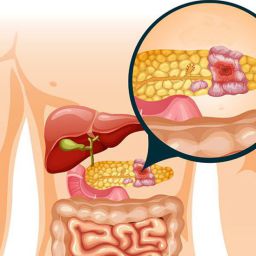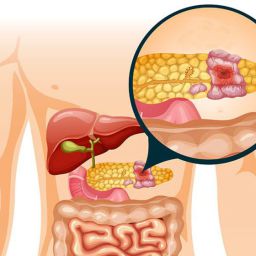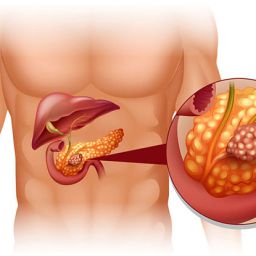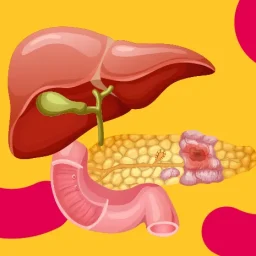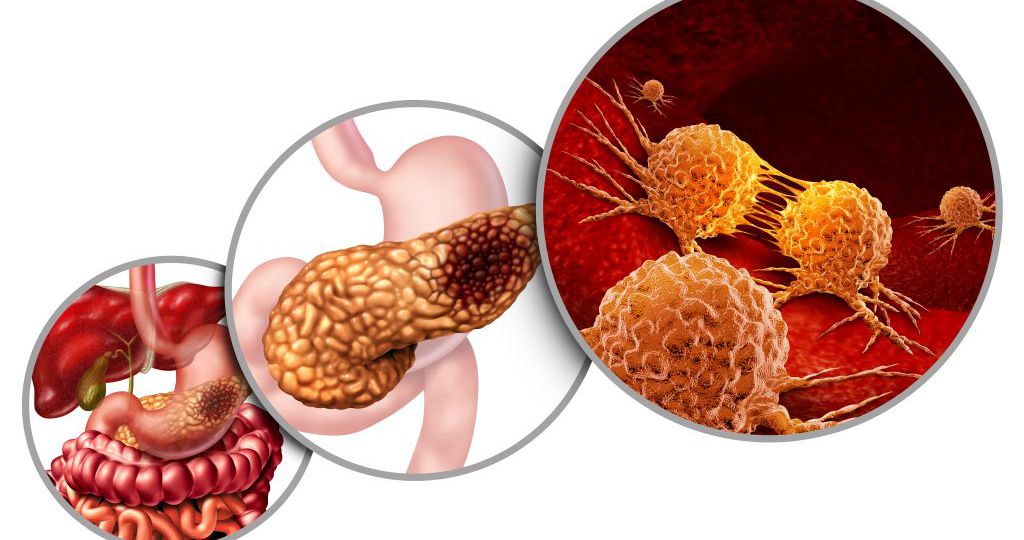
Pancreatic cancer is a serious and often aggressive form of cancer that originates in the pancreas, a vital organ responsible for producing insulin and enzymes that help digest food. Due to its location and the challenges in early detection, pancreatic cancer is often diagnosed at an advanced stage, making treatment more complex. However, surgery remains one of the most effective treatment options for patients who are diagnosed at an early or resectable stage.
In this article, we will explore the surgical intervention process for pancreatic cancer, detailing the types of surgeries available, the steps involved, and the potential benefits and risks of each procedure.
1. Overview of Pancreatic Cancer Surgery
Surgery for pancreatic cancer is typically considered when the tumor is localized to the pancreas and has not spread to distant organs. The primary goal of surgery is to remove the tumor and any affected tissues to achieve the best possible outcome, which may include complete remission or an improvement in quality of life.
However, not all patients with pancreatic cancer are candidates for surgery. Several factors, such as the location of the tumor, the stage of cancer, and the patient’s overall health, must be considered before deciding if surgery is a viable option.
2. Types of Surgery for Pancreatic Cancer
There are several types of surgical procedures used to treat pancreatic cancer, depending on the tumor’s size, location, and whether it has spread to surrounding tissues or lymph nodes. The primary surgical options include:
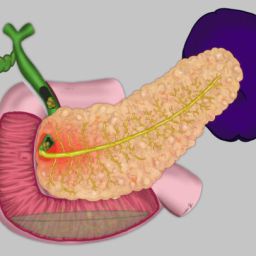
2.1. Pancreaticoduodenectomy (Whipple Procedure)
The Whipple procedure, also known as pancreaticoduodenectomy, is the most common surgery for pancreatic cancer when the tumor is located in the head of the pancreas. This complex and extensive surgery involves the removal of:
- The head of the pancreas
- The duodenum (the first part of the small intestine)
- The gallbladder
- The bile duct
- Part of the stomach
In some cases, lymph nodes around the pancreas and the small intestine may also be removed. After the tumor is excised, the remaining parts of the pancreas, bile duct, and digestive tract are reconnected. The Whipple procedure is a challenging surgery but can offer a chance for long-term survival for those with resectable pancreatic cancer.
2.2. Distal Pancreatectomy
A distal pancreatectomy is performed when the tumor is located in the body or tail of the pancreas. This surgery involves the removal of the tail or body of the pancreas, and in some cases, the spleen is also removed. If the cancer is confined to the pancreas, this surgery may offer a chance for a cure.
2.3. Total Pancreatectomy
In some cases, particularly when the cancer has spread to a large portion of the pancreas, a total pancreatectomy may be necessary. This surgery involves the removal of the entire pancreas, as well as the spleen, parts of the small intestine, and the bile duct. Afterward, patients will require lifelong insulin therapy, as the pancreas is no longer able to produce insulin. Total pancreatectomy is a more drastic measure but may be appropriate in select cases.
2.4. Laparoscopic Surgery
In certain cases, especially for small, localized tumors, laparoscopic surgery (a minimally invasive technique) may be used. This procedure involves making small incisions and using a camera (laparoscope) and specialized tools to remove the tumor. Laparoscopic surgery may offer benefits in terms of reduced recovery time, less pain, and a shorter hospital stay, although it is not suitable for all patients with pancreatic cancer.
3. Eligibility for Surgery
Not all pancreatic cancer patients are candidates for surgery. The eligibility largely depends on:
- The stage of the cancer: If the cancer has spread to nearby organs, lymph nodes, or distant parts of the body (metastasized), surgery may not be possible.
- The location of the tumor: Tumors located in areas of the pancreas that are difficult to access may not be surgically removable.
- The patient’s overall health: Because pancreatic cancer surgery is complex and requires a significant recovery period, patients need to be in good physical condition to withstand the procedure.
In some cases, patients may undergo chemotherapy or radiation therapy before surgery (neoadjuvant therapy) to shrink the tumor and make it more operable. In other cases, surgery may be performed after chemotherapy or radiation to remove any remaining cancer cells (adjuvant therapy).
4. The Surgical Process
The process of pancreatic cancer surgery typically follows several stages: preoperative assessment, the surgery itself, and postoperative care. Let’s break each stage down in more detail:
4.1. Preoperative Assessment
Before undergoing surgery, patients will undergo a series of tests to determine the extent of the cancer and assess their overall health. These tests may include:

- Imaging studies: CT scans, MRI scans, and sometimes PET scans are used to evaluate the tumor’s size, location, and potential spread.
- Blood tests: To check liver function, pancreas function, and overall health.
- Laparoscopy: A minimally invasive procedure in which a small camera is inserted into the abdomen to visually assess the pancreas and nearby structures.
- Consultations with specialists: These may include oncologists, nutritionists, and anesthesiologists to ensure the patient is in optimal condition for surgery.
The surgical team will use this information to determine if surgery is appropriate and which procedure will be most effective.
4.2. The Surgery Itself
Pancreatic cancer surgery is usually performed under general anesthesia. The patient will be unconscious and pain-free during the procedure. The surgery may take several hours, depending on the type of procedure being performed and the complexity of the tumor’s location.
For procedures like the Whipple procedure, the surgeon will make an incision in the upper abdomen to access the pancreas and remove the affected tissue. Once the tumor is removed, the remaining portions of the pancreas, bile duct, and digestive system will be reconnected.
4.3. Postoperative Care
After the surgery, patients will be moved to a recovery room and monitored closely. Postoperative care focuses on managing pain, preventing infection, and helping the patient recover from the anesthesia.
During the first few days after surgery, the patient will typically:
- Be given intravenous (IV) fluids and nutrition while their digestive system heals.
- Undergo monitoring for complications such as bleeding, infection, or leakage at the surgical site.
- Be encouraged to begin light physical activity, such as walking, to promote circulation and prevent blood clots.
Most patients will stay in the hospital for several days to a week following surgery, depending on their recovery progress. During this time, doctors will monitor for any complications and gradually reintroduce oral feeding.
4.4. Recovery and Follow-Up
Full recovery from pancreatic cancer surgery can take several weeks to months, depending on the extent of the procedure and the patient’s overall health. Physical therapy may be recommended to help regain strength and mobility.
Follow-up care is crucial to monitor for any signs of cancer recurrence and to manage potential complications. This may include regular imaging studies and blood tests, as well as additional chemotherapy or radiation therapy, depending on the type and stage of cancer.
5. Potential Risks and Complications
Like any major surgery, pancreatic cancer surgery carries risks, including:
- Infection: An infection can develop at the surgical site or in the abdominal cavity.
- Bleeding: There is a risk of bleeding during and after the procedure.
- Pancreatic leakage: In some cases, the reconnected parts of the pancreas or bile duct may leak, leading to further complications.
- Digestive issues: Removal of parts of the pancreas or digestive system may affect digestion, leading to malabsorption or difficulty digesting fats.
- Diabetes: If a significant portion of the pancreas is removed, patients may develop diabetes due to the loss of insulin production.
- Delayed gastric emptying: Some patients may experience difficulty with stomach emptying after the procedure, causing bloating and nausea.
5.1. Managing the Risks
While these risks exist, many patients recover without serious complications, especially when surgery is performed early and by an experienced surgical team. Preoperative optimization, including managing underlying health conditions and undergoing a thorough evaluation, can help minimize these risks.
Surgical intervention remains a cornerstone of treatment for pancreatic cancer, offering patients the best chance for long-term survival when the cancer is detected early and is resectable. The Whipple procedure, distal pancreatectomy, and total pancreatectomy are the main surgical options, each with its specific indications based on the tumor’s location and extent.
While the surgical process is complex and recovery can be challenging, many patients experience significant improvements in their quality of life and survival after surgery. As with any cancer treatment, early detection, personalized care, and a skilled medical team are essential in achieving the best outcomes.
If you or a loved one has been diagnosed with pancreatic cancer, it is essential to work closely with your oncologist and surgical team to determine the most appropriate course of action and understand the potential risks and benefits of surgery.