
The Immune System: A Brief Overview
Before diving into the specific effects of PIPAC, it’s important to understand the role of the immune system in cancer treatment. The immune system plays a crucial role in detecting and eliminating cancer cells. It does so through a sophisticated network of cells, proteins, and tissues. The immune system can broadly be divided into two types:
- Innate Immunity: This is the body’s first line of defense, responding rapidly to infections and abnormal cell growth, including cancer. Key players in innate immunity include macrophages, neutrophils, and natural killer (NK) cells.
- Adaptive Immunity: This is a more specific, targeted immune response that involves T cells and B cells. T cells can directly attack cancer cells, while B cells produce antibodies to neutralize foreign invaders.
Cancer cells are capable of evading immune detection through various mechanisms, including suppressing immune cell function and creating an immunosuppressive microenvironment. Chemotherapy treatments like PIPAC aim to enhance the immune system’s ability to recognize and combat these tumor cells.
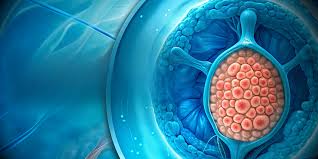
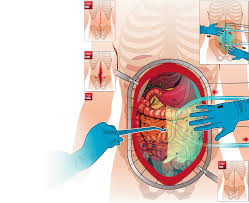
PIPAC: An Overview of the Treatment

PIPAC is a novel chemotherapy technique developed to treat peritoneal carcinomatosis, a condition where cancer cells spread to the peritoneal cavity. Unlike traditional intravenous chemotherapy, which disperses chemotherapy drugs throughout the body, PIPAC delivers chemotherapy directly into the peritoneum via an aerosolized spray under pressure. This method ensures that chemotherapy agents are concentrated in the areas where cancer is present, improving treatment efficacy while reducing side effects that typically occur with systemic chemotherapy.
PIPAC has shown promise in improving survival rates and quality of life for patients with advanced abdominal cancers. However, as with any cancer treatment, it comes with potential changes to the body’s immune system, both positive and negative.
Immune Response to PIPAC Treatment: The Mechanisms
Following PIPAC, several immune system changes can occur. These responses are mainly driven by the localized administration of chemotherapy agents, the pressure applied during the treatment, and the direct interaction between chemotherapy agents and cancer cells in the peritoneal cavity.
- Localized Inflammation and Immune Activation
One of the primary effects of PIPAC on the immune system is the induction of localized inflammation. The pressurized delivery of aerosolized chemotherapy drugs can trigger an inflammatory response in the peritoneum, which serves as a signal for the immune system to become activated. Inflammation is a key process in the body’s immune defense mechanisms. It helps recruit immune cells to the site of infection or injury, where they can work to neutralize harmful cells, including cancer cells.
Inflammatory cytokines, such as interleukins and tumor necrosis factor (TNF), are released in response to the chemotherapy treatment. These cytokines not only promote inflammation but also activate a cascade of immune responses that help recruit various immune cells, such as macrophages, dendritic cells, and T cells, to the tumor site.
- Macrophages and Dendritic Cells Recruitment
Macrophages, a type of white blood cell, play a crucial role in innate immunity. They are recruited to sites of inflammation where they ingest dead or dying cells, pathogens, and debris. After PIPAC treatment, macrophages can be activated by the inflammatory cytokines and serve as a bridge to the adaptive immune response by presenting cancer cell antigens to T cells. This helps the immune system recognize and attack tumor cells more effectively.
Dendritic cells, which act as antigen-presenting cells, are also recruited to the site of chemotherapy. These cells take up tumor antigens and present them to T cells, further stimulating the adaptive immune response. The recruitment and activation of macrophages and dendritic cells can significantly enhance the immune system’s ability to fight off cancer cells.
- Natural Killer (NK) Cells Activation
NK cells, a critical component of the innate immune system, play a role in directly killing cancer cells. In some studies, it has been shown that chemotherapy treatments like PIPAC can stimulate the activation of NK cells, helping them identify and kill tumor cells. NK cells are particularly effective in targeting abnormal cells that do not present normal “self” markers, such as cancer cells, which often express altered or absent surface molecules.
The activation of NK cells after PIPAC can contribute to an increased immune response against cancer cells, potentially improving treatment outcomes.
Immune System Suppression: The Downside of Chemotherapy
While PIPAC induces some immune activation, chemotherapy treatments are also known for their immunosuppressive effects. Chemotherapy drugs, including those used in PIPAC, can have toxic effects on both cancer cells and healthy immune cells, leading to a temporary suppression of the immune system. This immune suppression can make patients more vulnerable to infections, particularly after the treatment.
- Bone Marrow Suppression
Chemotherapy treatments like PIPAC can suppress the bone marrow, where immune cells are produced. This can result in decreased production of white blood cells, particularly neutrophils, which are essential for fighting infections. A reduced white blood cell count (leukopenia) increases the risk of bacterial, viral, and fungal infections, which can complicate recovery.
- T-cell Dysfunction
Although chemotherapy can activate certain immune cells, it can also have a suppressive effect on T cells, which play a central role in adaptive immunity. T cells are crucial for identifying and destroying cancer cells, but chemotherapy can impair their function or lead to a reduction in their numbers. This reduction can weaken the body’s ability to mount an effective immune response, potentially allowing residual cancer cells to evade detection.
- Immunosuppressive Microenvironment
Cancer cells are known to create an immunosuppressive microenvironment that protects them from immune detection. Chemotherapy can sometimes exacerbate this environment by killing both cancer cells and immune cells, which can dampen the body’s overall immune response. This can make it more difficult for the immune system to eradicate cancer cells fully, especially if there are remaining cancerous cells in the body.
Long-Term Immune Effects and Cancer Recurrence
One of the promising aspects of PIPAC is that it may have long-term effects on the immune system that contribute to cancer surveillance even after the treatment is over. The localized inflammation and immune activation caused by PIPAC may lead to prolonged immune responses, potentially increasing the body’s ability to detect and eliminate any remaining cancer cells.
Furthermore, the immune system may develop a form of “immune memory” that can help it recognize and attack any recurrent cancer in the future. This enhanced immune surveillance may reduce the risk of cancer recurrence after PIPAC treatment.
However, the long-term effects of PIPAC on immune function are still an area of ongoing research, and more studies are needed to fully understand how the treatment influences immune responses in the long run.
Managing Immune System Effects in PIPAC Treatment
Given the dual nature of immune activation and suppression following PIPAC treatment, it is crucial for medical professionals to closely monitor patients’ immune systems during and after the treatment. This can include:
- Monitoring White Blood Cell Count: Regular blood tests to track white blood cell counts can help identify any immune suppression early, allowing for timely intervention to prevent infections.
- Infection Prevention: Given the risk of infection due to reduced immune function, appropriate prophylactic measures, including the use of antibiotics or antifungals, may be necessary to protect the patient during recovery.
- Immunomodulatory Therapies: In some cases, immunomodulatory treatments may be used to boost the immune system and help maintain its ability to fight off infections while still being effective against cancer.
A Delicate Balance of Immune Activation and Suppression
The impact of PIPAC treatment on the immune system is a complex balance between immune activation and suppression. The localized inflammation triggered by the aerosolized chemotherapy can activate both innate and adaptive immune responses, helping the body target and destroy cancer cells. At the same time, chemotherapy can lead to immune suppression, particularly through the reduction in white blood cell counts and potential T-cell dysfunction.
The long-term effects of PIPAC on the immune system remain an area of active research, but early studies suggest that the treatment may enhance immune surveillance, potentially improving the body’s ability to detect and eliminate residual cancer cells. Close monitoring and management of immune function are essential for optimizing patient outcomes and minimizing the risks of infections and other complications.
In conclusion, while PIPAC offers an exciting and potentially life-saving treatment for peritoneal malignancies, understanding its effects on the immune system is key to ensuring its success and improving patient quality of life throughout the treatment process.

