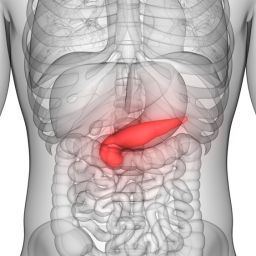
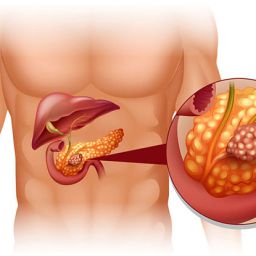
1. Understanding Quality of Life in Pancreatic Cancer Patients
Quality of life is a multifaceted concept that encompasses various aspects of an individual’s well-being, including physical health, emotional state, social functioning, and overall life satisfaction. For pancreatic cancer patients, improving QoL is often about managing the physical and emotional challenges of cancer treatment while maintaining as much independence and comfort as possible.
1.1 Factors Affecting Quality of Life in Pancreatic Cancer

- Physical Symptoms: Pancreatic cancer and its treatment often lead to fatigue, pain, weight loss, digestive issues, and loss of appetite, all of which can significantly affect QoL.
- Psychosocial Factors: The emotional impact of a cancer diagnosis can be profound, with many patients experiencing depression, anxiety, and stress, which can further diminish their overall well-being.
- Treatment Side Effects: Surgery, chemotherapy, radiation therapy, and other interventions come with side effects like nausea, fatigue, hair loss, and more, which can compromise the patient’s quality of life.
Understanding these factors is essential to creating a treatment plan that aims not only to treat the cancer but also to improve the patient’s quality of life throughout the process.
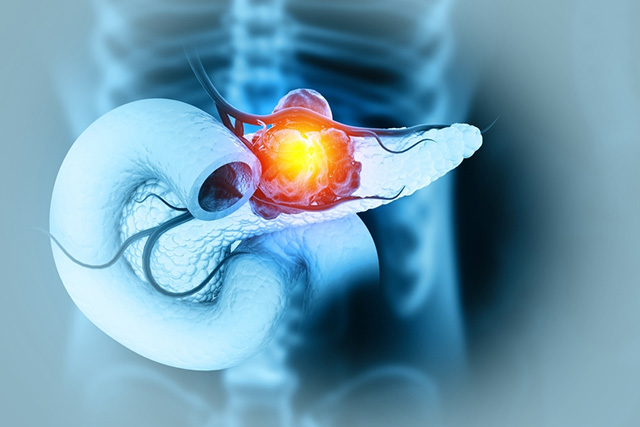
2. Medical Treatment Options and Their Impact on Quality of Life
The goal of pancreatic cancer treatment is to manage the cancer while improving symptoms and QoL. A multidisciplinary approach combining surgery, chemotherapy, radiation therapy, and targeted therapies can help patients live longer and feel better during their treatment. The following treatment options can influence quality of life in different ways:
2.1 Surgical Intervention
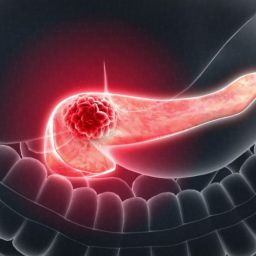
- Surgical Benefits: In some cases, surgery offers the best opportunity to improve survival and quality of life. Surgical procedures such as the Whipple procedure (pancreaticoduodenectomy) can remove tumors and relieve symptoms like jaundice and pain.
- Post-Surgical Recovery: While surgery can improve long-term outcomes, recovery can be challenging. However, with appropriate post-operative care, pain management, and physical therapy, many patients regain their independence and functional ability.
- Palliative Surgery: For patients with advanced cancer who cannot undergo curative surgery, palliative surgical options, such as bypass procedures, can help relieve blockages in the bile duct or intestines, improving digestion and comfort.
2.2 Chemotherapy and Targeted Therapy
- Symptom Control with Chemotherapy: Chemotherapy is a cornerstone of pancreatic cancer treatment. It can reduce tumor size, control pain, and alleviate other symptoms, contributing to improved quality of life.
- Targeted Therapies: Newer treatments that specifically target the cancer cells while minimizing damage to healthy tissues can help improve the QoL by reducing side effects like fatigue and gastrointestinal issues.
- Managing Side Effects of Chemotherapy: Managing the side effects of chemotherapy (e.g., nausea, vomiting, fatigue, and neuropathy) through medications, supportive care, and dietary adjustments can significantly improve a patient’s overall well-being.
2.3 Radiation Therapy
- Pain and Symptom Relief: Radiation therapy may be used to shrink tumors, especially in patients who are not candidates for surgery. It is effective in reducing pain caused by tumor pressure, making it a valuable tool for symptom management.
- Side Effects and Management: While radiation can improve quality of life by controlling pain and other symptoms, it may cause fatigue, skin irritation, and digestive issues, which can be managed with supportive care.
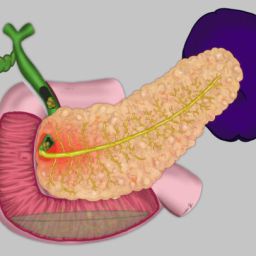
3. Nutritional Support: A Key Component of Quality of Life
Nutrition plays a critical role in supporting overall health and well-being in pancreatic cancer patients. Malnutrition, weight loss, and digestive issues are common, and managing these can significantly improve a patient’s quality of life.
3.1 The Role of Diet in Managing Symptoms
- Managing Malabsorption: As pancreatic cancer impairs the pancreas’s ability to secrete digestive enzymes, patients may require enzyme replacement therapy (ERT) to ensure proper digestion and nutrient absorption.
- High-Calorie, High-Protein Diets: A focus on nutrient-dense, high-calorie foods can help combat weight loss and improve energy levels. Protein-rich foods are essential for healing and maintaining muscle mass, which can be compromised during treatment.
- Small, Frequent Meals: For patients experiencing reduced appetite or early satiety, small, frequent meals may be easier to tolerate than larger portions.
3.2 Hydration and Electrolyte Balance
- Hydration: Staying hydrated is crucial for maintaining energy and avoiding dehydration, especially for patients undergoing chemotherapy or radiation. Electrolyte drinks or hydration solutions can also help replenish essential minerals.
- Managing Digestive Issues: Patients with pancreatic cancer often experience issues such as diarrhea, constipation, and bloating, which can be alleviated with proper dietary adjustments, medications, and hydration.
4. Physical Activity and Rehabilitation
Physical activity is essential for maintaining strength, reducing fatigue, and improving overall well-being in pancreatic cancer patients. While physical activity levels will vary depending on the patient’s condition, incorporating gentle exercises into the daily routine can yield significant benefits.
4.1 The Importance of Exercise
- Improved Muscle Strength and Endurance: Regular physical activity helps prevent muscle wasting, which is common in cancer patients, and supports better overall mobility.
- Reduced Fatigue: Even moderate physical activity can reduce fatigue, a common complaint among pancreatic cancer patients undergoing treatment.
- Improved Mental Health: Exercise is also beneficial for mental health, reducing anxiety and depression, which are prevalent in cancer patients.
4.2 Rehabilitation and Physical Therapy
- Recovery from Surgery: After surgical interventions, physical therapy and rehabilitation are important for improving mobility and restoring strength.
- Pain Management: Physical therapy can help manage cancer-related pain by improving posture, flexibility, and overall movement.
5. Psychosocial Support and Mental Well-being
Living with cancer takes a significant emotional toll, and addressing the mental health needs of pancreatic cancer patients is critical for improving quality of life. Support from family, friends, and healthcare providers is essential.
5.1 Psychological Support Services
- Counseling and Therapy: Individual or group therapy sessions can help patients cope with the emotional and mental challenges of their diagnosis and treatment. Cognitive-behavioral therapy (CBT) and mindfulness practices have been shown to help manage stress, anxiety, and depression.
- Support Groups: Connecting with others who are experiencing similar challenges can provide emotional support and reduce feelings of isolation.
- Palliative Psychological Support: Palliative care teams often include mental health professionals who focus on reducing emotional distress during advanced stages of the disease.
5.2 Family and Caregiver Support
- Caregiver Assistance: Caring for a loved one with pancreatic cancer can be physically and emotionally demanding. Providing caregivers with resources, training, and support can improve their well-being and the overall care they provide.
- Family Counseling: Family members may also benefit from counseling services to help them cope with the emotional strain of caregiving and dealing with a loved one’s diagnosis.
6. Integrative and Complementary Therapies
In addition to conventional medical treatments, many pancreatic cancer patients explore complementary therapies that can help enhance their quality of life. While these therapies should always be used in conjunction with conventional treatments, they can provide additional relief and comfort.
6.1 Acupuncture and Acupressure
- Acupuncture has been used to reduce pain, nausea, and fatigue, and may help improve the body’s overall balance and energy levels. It is often used in conjunction with conventional therapies to alleviate treatment side effects.
6.2 Massage and Aromatherapy
- Massage Therapy: Gentle massage can help alleviate pain, reduce stress, and improve relaxation.
- Aromatherapy: Essential oils such as lavender, peppermint, and chamomile may help reduce anxiety, nausea, and promote relaxation.
6.3 Mind-Body Techniques
- Mindfulness and Meditation: Mindfulness practices and meditation techniques can help reduce anxiety and improve emotional well-being, making them effective tools in cancer care.
- Yoga and Relaxation Exercises: Yoga can improve flexibility, strength, and mental clarity, helping patients feel more centered during treatment.
7. A Holistic Approach to Improving Quality of Life
Improving the quality of life for pancreatic cancer patients requires a holistic approach that addresses both the physical and emotional aspects of the disease. By combining medical treatments with nutritional support, physical activity, psychological care, and complementary therapies, patients can better manage symptoms and maintain a higher level of well-being during their cancer journey. Working closely with a multidisciplinary team of healthcare providers is essential to create an individualized care plan that enhances both the quantity and quality of life for pancreatic cancer patients.