
Understanding the Parathyroid Glands and Calcium Regulation
The parathyroid glands are small, pea-sized glands located behind the thyroid gland in the neck. There are usually four parathyroid glands, and their primary function is to regulate calcium and phosphate levels in the body. They do so by releasing parathyroid hormone (PTH), which controls the levels of calcium in the blood through its effects on the bones, kidneys, and intestines.
When the parathyroid glands become overactive, they can produce too much PTH, which leads to elevated calcium levels in the blood. This condition is called hyperparathyroidism and can result in hypercalcemia (high blood calcium levels).
There are two main types of hyperparathyroidism:
- Primary Hyperparathyroidism: This occurs when one or more of the parathyroid glands develop a tumor (adenoma) or become enlarged, leading to an overproduction of PTH.
- Secondary Hyperparathyroidism: This type is caused by another condition, such as chronic kidney disease, that leads to low calcium levels, prompting the parathyroid glands to overcompensate and produce excessive PTH.
Regardless of the type of hyperparathyroidism, the primary goal of treatment is to reduce elevated calcium levels, often through parathyroid surgery. However, managing calcium levels before surgery is critical to reduce the risks associated with hypercalcemia and improve patient outcomes.
Why Is Managing Calcium Levels Before Parathyroid Surgery Important?
High calcium levels can cause a range of symptoms, including:

- Fatigue
- Nausea and vomiting
- Constipation
- Increased thirst and frequent urination
- Bone pain and muscle weakness
- Kidney stones
- Cognitive changes, such as confusion or memory problems
In severe cases, hypercalcemia can lead to life-threatening complications such as cardiac arrhythmias (irregular heartbeats), kidney failure, or coma. Therefore, it is crucial to manage calcium levels before surgery to reduce these risks.
Additionally, high calcium levels can affect the outcome of the surgery. Elevated calcium can lead to difficulties in anesthesia management, and it may also impair the healing process after surgery. Ensuring that calcium levels are well-controlled prior to surgery can improve the patient’s safety during the operation and speed up recovery.
Methods of Managing Calcium Levels Before Surgery
There are several methods used to manage calcium levels before parathyroid surgery. These methods aim to lower calcium levels gradually and safely, reducing the risk of complications associated with hypercalcemia.
1. Hydration Therapy
One of the first steps in managing hypercalcemia is to increase fluid intake. Dehydration can exacerbate the symptoms of high calcium levels, so intravenous (IV) hydration is often used to help dilute the calcium in the blood and improve kidney function.
IV fluids, typically saline, help to flush excess calcium from the body through the kidneys, thereby reducing blood calcium levels. This process can take several hours or days, depending on the severity of hypercalcemia. Proper hydration helps improve kidney function and also alleviates some of the common symptoms of hypercalcemia, such as fatigue, nausea, and dehydration.
2. Medications
In addition to hydration therapy, medications are commonly used to lower calcium levels before surgery. These medications work by either decreasing the release of calcium from the bones or enhancing calcium excretion from the kidneys. Some of the most common medications include:
- Bisphosphonates: These drugs, such as zoledronic acid (Zometa) or pamidronate, help inhibit the release of calcium from the bones by suppressing osteoclast activity. Bisphosphonates are often used for patients with severe hypercalcemia or those who have been symptomatic for a long time.
- Calcitonin: Calcitonin is a hormone that helps lower calcium levels by inhibiting the activity of osteoclasts (the cells responsible for breaking down bone tissue). It can provide quick relief from hypercalcemia, although its effects are typically short-lived.
- Steroids: Corticosteroids, such as prednisone, may be used to treat hypercalcemia in certain cases, especially when it is associated with granulomatous diseases or vitamin D toxicity. Steroids can help reduce calcium levels by decreasing the absorption of calcium from the intestines.
- Furosemide (Lasix): A diuretic medication that can increase urine output and help the kidneys excrete excess calcium. However, it is typically used with caution, as it can lead to dehydration or electrolyte imbalances.
- Phosphate Therapy: In some cases, intravenous phosphate may be used to bind calcium and help reduce blood calcium levels. This method is typically reserved for more severe cases of hypercalcemia.
3. Dialysis
For patients with kidney problems or severe hypercalcemia that cannot be managed with medications and hydration alone, dialysis may be required. Dialysis is a procedure that helps remove excess calcium and other waste products from the blood. It is typically used when other methods are ineffective or if the patient has a compromised kidney function.
4. Dietary Adjustments
Although dietary changes alone are not sufficient to lower calcium levels dramatically, they can play a supportive role in managing hypercalcemia before surgery. Patients may be advised to reduce their intake of calcium-rich foods (such as dairy products, leafy greens, and fortified foods) and avoid calcium supplements. Additionally, consuming a diet that supports kidney function, such as low-sodium and low-protein foods, can be beneficial.
5. Monitor and Adjust Calcium Levels Regularly
Throughout the process of lowering calcium levels, it is essential to monitor calcium levels regularly. Blood tests will be conducted frequently to track the patient’s progress. These tests will help guide the adjustments in treatment and ensure that calcium levels are being lowered effectively without dropping too quickly, which could cause other health problems.
Preparing for Surgery: The Role of Preoperative Management
Once calcium levels have been sufficiently managed and the patient is stable, they will be cleared for parathyroid surgery. Preoperative preparation involves not only managing calcium but also ensuring that the patient is healthy enough to undergo surgery. This may include:
- Reviewing medical history and discussing any underlying health conditions, such as heart disease, which may require special consideration during the surgery.
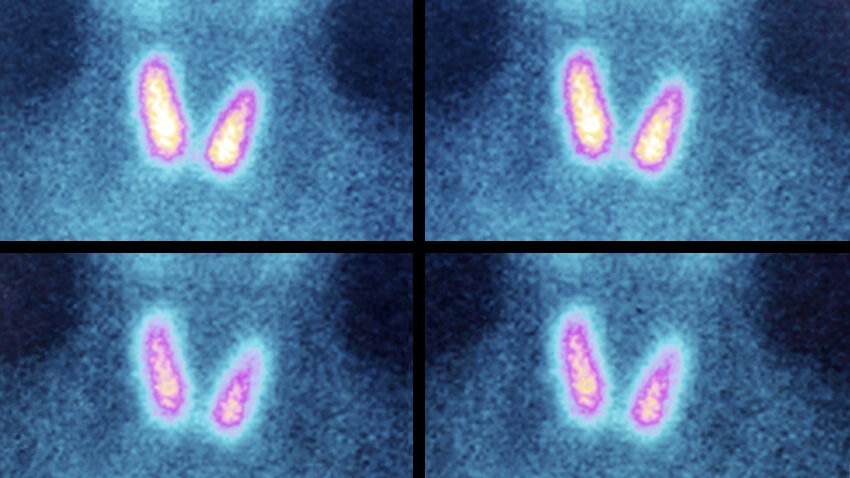
- Preoperative imaging, such as an ultrasound, sestamibi scan, or CT scan, to locate the overactive parathyroid gland(s) and guide the surgeon.
- Anesthesia assessment, to determine the best approach to anesthesia and minimize any risks associated with high calcium levels during surgery.
Managing calcium levels before parathyroid surgery is a critical step in preparing patients for a safe and successful operation. Hypercalcemia caused by hyperparathyroidism can lead to a variety of symptoms and complications, but with the appropriate interventions, calcium levels can be controlled effectively.
Hydration therapy, medications such as bisphosphonates and calcitonin, dietary adjustments, and, in some cases, dialysis are all essential tools in managing high calcium levels before surgery. By addressing hypercalcemia early and carefully monitoring calcium levels, healthcare providers can minimize risks and improve the patient’s surgical outcomes.
For individuals undergoing parathyroid surgery, it is essential to work closely with an experienced medical team to ensure that calcium levels are well-controlled before surgery. This careful management not only reduces risks but also aids in faster recovery and better long-term health outcomes.

