1. Acute Pancreatitis Is Always Caused by Alcohol Consumption
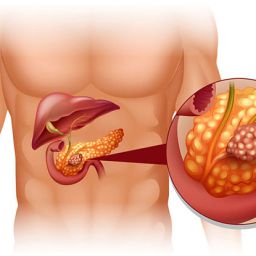
One of the most pervasive misconceptions about acute pancreatitis is that it is solely caused by excessive alcohol consumption. While alcohol is a significant risk factor, it is not the only cause. In fact, a variety of other conditions can trigger acute pancreatitis, such as:
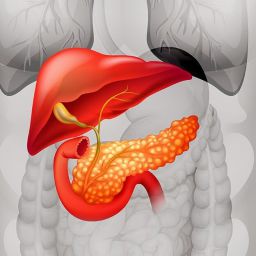
- Gallstones: Gallstones can block the bile duct, which can lead to pancreatitis.
- Medications: Certain medications, like corticosteroids, can induce pancreatitis in some individuals.
- Infections: Viral infections like mumps or coxsackievirus can lead to pancreatitis.
- Trauma or Surgery: Injuries to the abdomen or surgery near the pancreas can cause inflammation.
- Hypertriglyceridemia: Extremely high levels of triglycerides in the blood can increase the risk of developing acute pancreatitis.
- Genetic Conditions: Inherited genetic disorders can also play a role in the onset of acute pancreatitis.
While chronic alcohol abuse is a significant risk factor, it is essential to understand that acute pancreatitis can develop in individuals who do not drink alcohol at all.
2. Acute Pancreatitis Is Always a Fatal Condition
Another common misconception is that acute pancreatitis is always a life-threatening disease. While acute pancreatitis can be severe and, in some cases, lead to complications such as organ failure or infection, the majority of people with acute pancreatitis will recover fully with appropriate treatment.
The prognosis largely depends on the severity of the condition, with most mild cases resolving with supportive care (rest, fluids, and pain management). However, severe cases may require hospitalization, and in some instances, surgical intervention or intensive care may be necessary.
It’s important to note that early diagnosis, medical intervention, and proper treatment significantly improve the chances of recovery. Therefore, while acute pancreatitis can be serious, it is not necessarily fatal.
3. The Symptoms of Acute Pancreatitis Are Always Obvious
Many people believe that the symptoms of acute pancreatitis are always easy to recognize. However, the symptoms can vary widely from person to person and sometimes mimic other conditions. The most common symptom is severe abdominal pain, which typically occurs in the upper abdomen and can radiate to the back. Other symptoms may include:
- Nausea and vomiting
- Fever
- Rapid pulse
- Swelling or tenderness in the abdomen
However, not all cases of acute pancreatitis present with the same symptoms. Some people may experience mild discomfort, while others may have more pronounced symptoms. In rare cases, symptoms may be less obvious, leading to delayed diagnosis. Furthermore, some individuals with mild pancreatitis may not exhibit classic signs, making it crucial to seek medical attention if abdominal pain is persistent or severe.
4. Acute Pancreatitis Only Affects the Elderly

While acute pancreatitis is more commonly diagnosed in individuals over the age of 50, it is by no means limited to the elderly. Acute pancreatitis can affect people of all ages, including children and young adults. In fact, younger individuals may be at increased risk due to certain genetic predispositions or conditions like hypertriglyceridemia.
For instance, genetic mutations, bile duct abnormalities, or high cholesterol can predispose younger individuals to acute pancreatitis. It’s important to recognize that age is not the sole determining factor in the development of this condition, and people of all ages should be vigilant for symptoms and risk factors.
5. Once You Have Acute Pancreatitis, You’ll Always Be at Risk
While it is true that individuals who have experienced acute pancreatitis once are at a higher risk of developing it again, it is not inevitable. Lifestyle changes, such as avoiding alcohol and adopting a healthy diet, can significantly reduce the likelihood of recurrence.
For example, if acute pancreatitis was triggered by gallstones, removing the gallbladder can eliminate that particular risk factor. Likewise, for individuals with high triglycerides or other metabolic conditions, managing these factors through lifestyle changes and medication can greatly reduce the risk of a repeat episode.
It’s essential for people who have had acute pancreatitis to work closely with their healthcare providers to monitor their health and make necessary lifestyle changes to prevent recurrence.
6. People with Acute Pancreatitis Should Avoid All Food and Drink Completely
A common misconception about the treatment of acute pancreatitis is that individuals should refrain from consuming any food or fluids until the condition resolves completely. While it is true that patients may be instructed to fast during the acute phase to allow the pancreas to rest and heal, this is only a temporary measure.
As the condition improves, doctors often gradually introduce clear liquids and light, easily digestible foods into the patient’s diet. The idea is to reintroduce nutrition slowly, allowing the pancreas to function without causing additional strain.
In more severe cases, nutrition may be provided through an intravenous line (IV) or feeding tube until the patient is stable enough to eat normally. It is important for patients to follow their healthcare provider’s advice on diet and fluid intake during the recovery process.
7. Acute Pancreatitis and Chronic Pancreatitis Are the Same
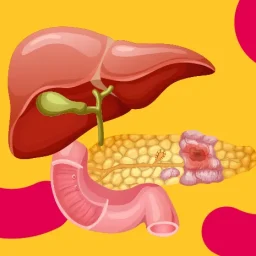
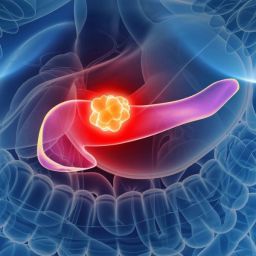
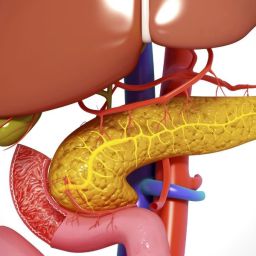
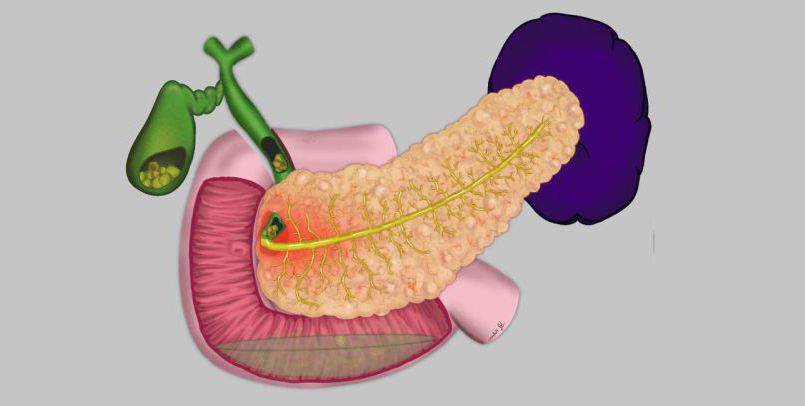
Though acute and chronic pancreatitis share similar symptoms and both affect the pancreas, they are distinct conditions. Acute pancreatitis is a sudden, short-term inflammation, while chronic pancreatitis is a long-term, ongoing condition that results from repeated episodes of inflammation.
Chronic pancreatitis can lead to permanent damage to the pancreas, resulting in a loss of pancreatic function. It is often associated with long-term alcohol use, smoking, or genetic predispositions. Unlike acute pancreatitis, chronic pancreatitis can lead to digestive issues such as malabsorption, and insulin-dependent diabetes, and may require ongoing management.
Acute pancreatitis is a serious but often misunderstood condition. Clearing up the common misconceptions about its causes, symptoms, treatment, and prognosis is essential to fostering better understanding and improving outcomes for those affected. By providing accurate information, we can help people make informed decisions about their health and seek the necessary medical attention when needed.
If you or someone you know is experiencing symptoms of acute pancreatitis, it’s crucial to seek medical help promptly. Early diagnosis and appropriate treatment can significantly improve recovery chances and minimize complications. Through education and awareness, we can better manage the risks and realities of acute pancreatitis and improve the quality of life for those affected.