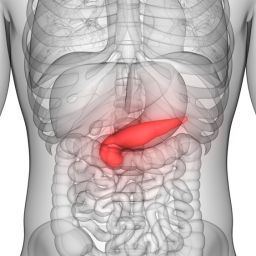
1. The Role of the Pancreas in Digestion
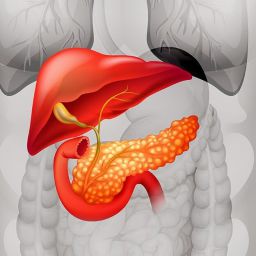
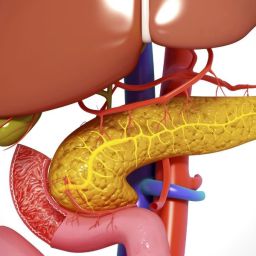
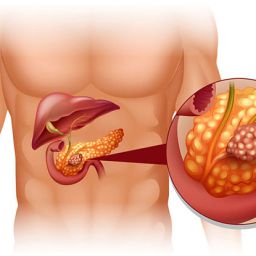
To understand how chronic pancreatitis leads to digestive problems, it’s essential to first look at the pancreas’ role in digestion. The pancreas is a vital organ located behind the stomach that performs both endocrine and exocrine functions. The exocrine function is particularly important for digestion, as the pancreas produces enzymes that help break down carbohydrates, fats, and proteins.
The key digestive enzymes produced by the pancreas include:
- Amylase: Breaks down carbohydrates into sugars.
- Lipase: Breaks down fats into fatty acids and glycerol.
- Proteases (e.g., trypsin): Break down proteins into amino acids.
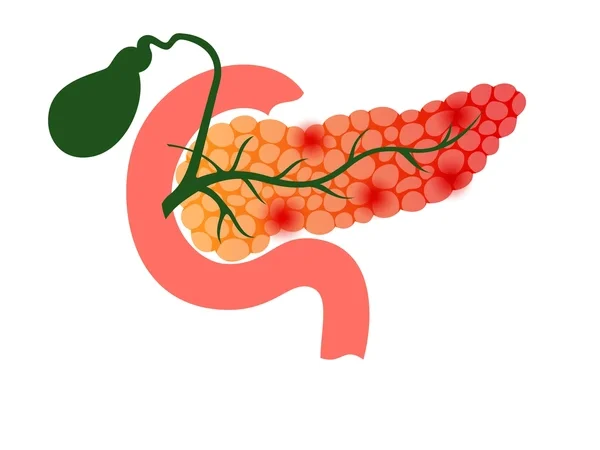
When the pancreas becomes inflamed, as in chronic pancreatitis, its ability to produce these digestive enzymes is compromised, leading to significant digestive issues.
2. Enzyme Deficiency: A Key Factor in Digestive Problems
One of the primary causes of digestive problems in chronic pancreatitis is enzyme deficiency. As the inflammation progresses and pancreatic tissue is damaged, the pancreas struggles to produce sufficient amounts of digestive enzymes. This results in exocrine pancreatic insufficiency (EPI), a condition where the pancreas cannot release enough enzymes to properly digest food.
Enzyme deficiency can lead to a variety of digestive problems, including:
- Malabsorption: Without enough digestive enzymes, the body cannot properly absorb nutrients, especially fats. This can result in weight loss, malnutrition, and deficiencies in essential vitamins (such as fat-soluble vitamins A, D, E, and K).
- Steatorrhea: This is the presence of undigested fat in the stool, leading to fatty, bulky, and foul-smelling stools.
- Diarrhea: Incomplete digestion of food can result in diarrhea, which is often watery and may be accompanied by bloating and discomfort.
Managing enzyme deficiency through pancreatic enzyme replacement therapy (PERT) is critical for controlling these symptoms and improving digestion in people with chronic pancreatitis.
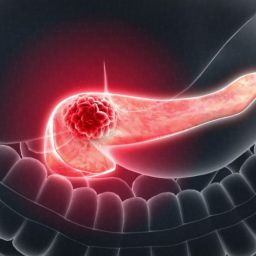
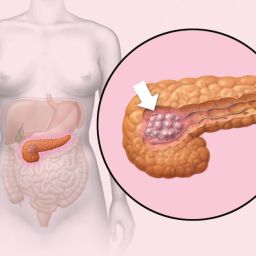
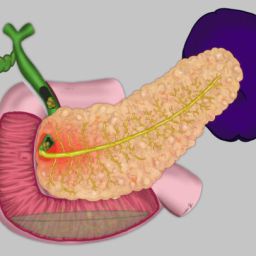
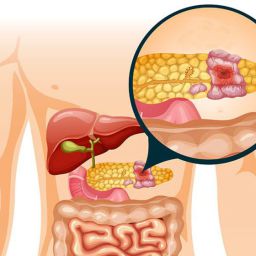
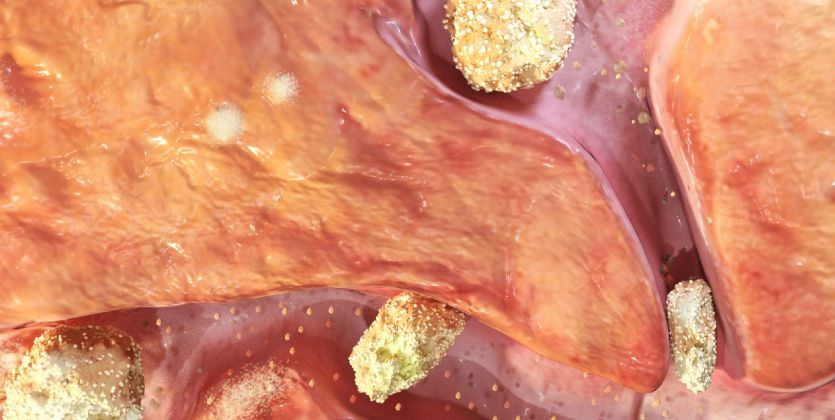
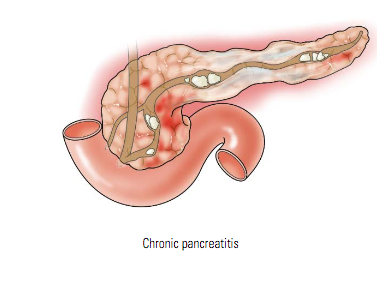
3. Pancreatic Scarring and Ductal Obstruction
As chronic pancreatitis progresses, the pancreatic tissue becomes scarred (fibrotic) and the ducts that transport enzymes and digestive juices may become obstructed. This can further exacerbate digestive problems in several ways:
- Reduced Enzyme Secretion: Scarring and ductal obstruction make it more difficult for the pancreas to secrete enzymes into the small intestine. This leads to reduced enzyme availability for digestion and worsens malabsorption.
- Bile Duct Blockage: In some cases, chronic pancreatitis can also affect the bile ducts, leading to a buildup of bile. This can impair the digestion of fats and lead to jaundice, an additional complication.
- Increased Risk of Pancreatic Cancer: Long-term inflammation and scarring can increase the risk of developing pancreatic cancer, which can further disrupt digestive function and complicate the management of chronic pancreatitis.
4. Altered Gut Motility
Chronic pancreatitis can also affect gut motility, or the ability of the intestines to contract and move food through the digestive tract. This disruption can lead to several digestive issues, including:
- Delayed Gastric Emptying: When the stomach takes too long to empty its contents into the small intestine, individuals may experience bloating, nausea, and feelings of fullness after eating.
- Small Bowel Bacterial Overgrowth (SIBO): Disruptions in normal gut motility can create an environment that promotes the overgrowth of bacteria in the small intestine. This condition, known as SIBO, can result in symptoms such as bloating, diarrhea, and malabsorption.
- Constipation: In some cases, individuals with chronic pancreatitis may also experience constipation due to slowed gut motility.
5. Impact on the Endocrine Function of the Pancreas
In addition to its exocrine function (producing digestive enzymes), the pancreas also has an endocrine function. The pancreas releases insulin and glucagon into the bloodstream to help regulate blood sugar levels. In chronic pancreatitis, the damage to the pancreas can lead to impaired endocrine function, resulting in diabetes. This condition, known as pancreatogenic diabetes or type 3c diabetes, can further complicate digestive health.
The connection between chronic pancreatitis and diabetes can affect digestion in several ways:
- Slower Digestion: High blood sugar levels can affect the nerves in the digestive tract, leading to slower digestion.
- Malnutrition: Uncontrolled diabetes can lead to weight loss and malnutrition, further compounding the digestive issues caused by chronic pancreatitis.
6. Dietary Factors and Their Role in Digestive Problems
Diet plays a significant role in managing chronic pancreatitis and its digestive complications. Certain dietary habits and food choices can either exacerbate or alleviate symptoms. Individuals with chronic pancreatitis may experience digestive problems if they consume foods that are difficult to digest or that irritate the pancreas.
Some factors to consider include:
- High-Fat Foods: Fats are particularly challenging for individuals with chronic pancreatitis to digest. Fatty foods can worsen malabsorption and cause symptoms like bloating and diarrhea. A low-fat diet is often recommended to ease digestive distress.
- Spicy Foods: Spicy foods can irritate the digestive tract and worsen symptoms like nausea and abdominal pain. Avoiding these foods can help manage digestive problems.
- Large Meals: Eating large meals can overwhelm the digestive system and increase the strain on the pancreas. Smaller, more frequent meals are often recommended to reduce digestive discomfort.
- Alcohol: Alcohol is a major risk factor for the development and worsening of chronic pancreatitis. Even small amounts of alcohol can trigger flare-ups and worsen digestive symptoms.
7. Managing Digestive Problems in Chronic Pancreatitis
There are several strategies that individuals with chronic pancreatitis can employ to manage their digestive problems and improve their quality of life:
- Pancreatic Enzyme Replacement Therapy (PERT): Taking enzyme supplements can help replace the digestive enzymes the pancreas is no longer producing, aiding digestion and reducing malabsorption.
- Dietary Modifications: Following a low-fat, high-protein, and nutrient-dense diet can help manage digestive issues. A dietitian can assist in creating a meal plan tailored to individual needs.
- Small, Frequent Meals: Eating smaller meals throughout the day can prevent the pancreas from being overwhelmed and make digestion easier.
- Managing Diabetes: If diabetes has developed as a result of chronic pancreatitis, effective blood sugar management is critical for overall digestive health.
- Pain Management: Chronic pancreatitis often causes severe abdominal pain, which can interfere with digestion. Pain management through medications, nerve blocks, or other interventions is essential for improving digestion and overall well-being.
- Vitamin and Mineral Supplementation: Malabsorption can lead to vitamin deficiencies, so supplementation may be necessary to ensure that individuals get enough essential nutrients.
Chronic pancreatitis can significantly impact digestion, leading to a range of digestive problems due to the loss of pancreatic function, enzyme deficiencies, and complications such as ductal obstruction, altered gut motility, and diabetes. However, with proper management, including enzyme replacement therapy, dietary adjustments, and pain control, individuals with chronic pancreatitis can reduce digestive issues and improve their quality of life.
It is crucial for individuals with chronic pancreatitis to work closely with their healthcare providers to create a personalized treatment plan that addresses their specific needs and helps manage their digestive symptoms effectively. Education, proactive management, and lifestyle changes can help individuals living with chronic pancreatitis navigate the challenges posed by digestive problems and lead healthier, more fulfilling lives.