1. The Connection Between Chronic Pancreatitis and Stress
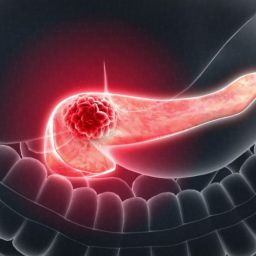
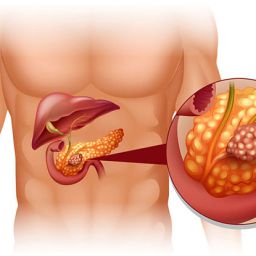
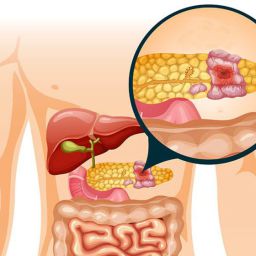
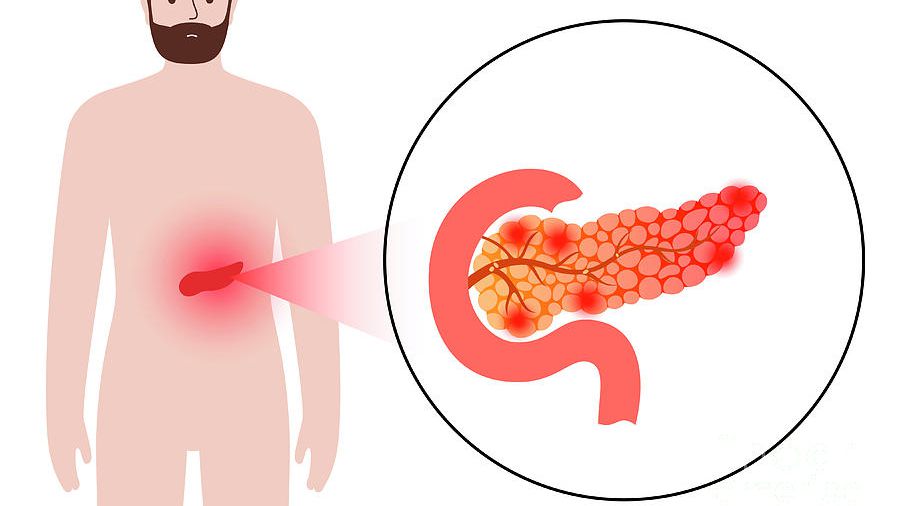
Chronic pancreatitis is a long-term disease that can lead to chronic abdominal pain, digestive issues, malnutrition, and diabetes. As patients struggle with these symptoms, they may also experience psychological distress, anxiety, and depression. The relationship between chronic illness and stress is well-established, with studies showing that individuals with chronic conditions like pancreatitis are more likely to experience elevated stress levels.
Stress is the body’s response to external pressures, whether they are physical, emotional, or psychological. In the case of chronic pancreatitis, constant pain, dietary restrictions, medical treatments, and the fear of disease progression all contribute to an increase in stress levels. Over time, chronic stress can worsen physical symptoms, creating a vicious cycle of discomfort and mental health struggles.
2. How Stress Affects the Body and Pancreas
Stress can have both direct and indirect effects on the body, and in individuals with chronic pancreatitis, these effects may compound existing symptoms. The body’s stress response involves the activation of the sympathetic nervous system, which triggers the release of stress hormones such as cortisol and adrenaline.
These hormones can affect various physiological processes, including:

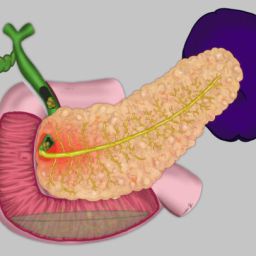
- Increased Inflammation: Chronic stress can worsen inflammation in the body, potentially aggravating the inflammation in the pancreas and leading to further damage to the organ. This can exacerbate symptoms such as abdominal pain and discomfort.
- Digestive Problems: Stress can impair digestion by affecting gut motility, increasing the likelihood of bloating, indigestion, and diarrhea. Individuals with chronic pancreatitis already face digestive difficulties due to enzyme insufficiency, and stress can worsen these issues.
- Pain Sensitivity: Research has shown that stress can amplify pain sensitivity, making individuals with chronic pancreatitis more vulnerable to experiencing intense or prolonged episodes of pain.
- Immune Function: Chronic stress can weaken the immune system, reducing the body’s ability to fight infections and heal. This is particularly concerning for people with chronic pancreatitis, as they are at higher risk of infections and complications related to the disease.
Additionally, high levels of stress can increase the production of stomach acid, potentially leading to ulcers or worsening existing gastrointestinal issues.
3. Psychological Effects of Chronic Pancreatitis
The physical symptoms of chronic pancreatitis are often accompanied by a range of psychological challenges, including anxiety, depression, and fear. These mental health concerns can significantly reduce an individual’s quality of life and complicate the management of the disease.
Anxiety and Chronic Pancreatitis
Many individuals with chronic pancreatitis experience heightened levels of anxiety, often related to the uncertainty of their condition. The unpredictable nature of flare-ups, the fear of complications, and the ongoing struggle with chronic pain can create a constant sense of worry. Anxiety can also exacerbate physical symptoms by increasing muscle tension and further stimulating the body’s stress response.
Depression and Chronic Illness
Depression is another common psychological effect of chronic pancreatitis. The ongoing pain, digestive issues, and lifestyle restrictions can lead to feelings of hopelessness, frustration, and sadness. Depression may also be triggered by the inability to engage in normal activities, work, or social interactions due to the physical limitations of chronic pancreatitis. The emotional toll of living with a chronic illness can contribute to a decreased quality of life and may lead to difficulty in adhering to treatment plans.
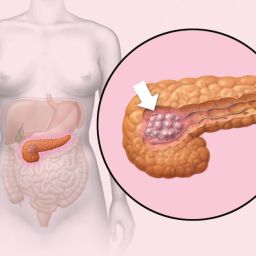
Fear of Disease Progression and Complications
Living with chronic pancreatitis also involves a constant fear of disease progression and potential complications, such as pancreatic cancer or the development of diabetes. This fear can create a sense of helplessness and increase psychological distress, particularly if the individual has experienced episodes of acute pancreatitis or is facing ongoing treatment.
4. Impact of Stress on Treatment Adherence
The mental health challenges associated with chronic pancreatitis can also impact a person’s ability to adhere to their treatment regimen. High stress levels, anxiety, and depression can make it difficult for individuals to focus on managing their condition and following medical advice. For example:
- Skipping Medications: Depression or anxiety may make it harder for individuals to consistently take prescribed medications, including painkillers or enzyme replacement therapy.
- Avoiding Dietary Guidelines: The dietary restrictions associated with chronic pancreatitis, such as a low-fat diet and avoiding alcohol, may be challenging to adhere to, especially when stress or emotional struggles lead to unhealthy coping mechanisms like overeating or binge drinking.
- Neglecting Self-Care: When stress and depression take hold, individuals may neglect other aspects of their health, such as regular check-ups, physical activity, or managing other conditions like diabetes. This can lead to further complications and a worsening of both mental and physical health.
5. Strategies for Managing Stress and Improving Mental Health
Addressing the psychological aspects of chronic pancreatitis is just as important as managing the physical symptoms. By incorporating stress management techniques and mental health support, individuals can improve their overall well-being and quality of life.
Psychological Counseling and Therapy
Seeking professional help from a psychologist or counselor can provide individuals with the tools to cope with the emotional challenges of chronic pancreatitis. Cognitive behavioral therapy (CBT) is particularly effective in treating anxiety and depression, helping individuals change negative thought patterns and build healthier coping strategies.
Support Groups
Support groups for people with chronic pancreatitis or other chronic illnesses can provide a sense of community and reduce feelings of isolation. Sharing experiences with others facing similar challenges can help individuals feel understood and less alone in their struggles. Support groups can also provide valuable insights into effective coping mechanisms and treatment options.
Mindfulness and Relaxation Techniques
Practices such as mindfulness meditation, yoga, and deep breathing exercises can help reduce stress and improve emotional well-being. These techniques help individuals focus on the present moment, calm their minds, and manage pain more effectively. Regular practice of mindfulness and relaxation exercises has been shown to reduce anxiety and depression in people with chronic health conditions.
Chronic pancreatitis is a challenging condition that affects not only the body but also the mind. The stress associated with the disease can worsen physical symptoms, create a cycle of pain and discomfort, and contribute to anxiety, depression, and other psychological issues. Addressing both the physical and psychological aspects of chronic pancreatitis is essential for improving the overall quality of life.
Stress management, mental health support, and lifestyle modifications are key components of a comprehensive treatment plan for chronic pancreatitis. By reducing stress and improving emotional well-being, individuals with chronic pancreatitis can better manage their condition, adhere to treatment plans, and lead healthier, more fulfilling lives.