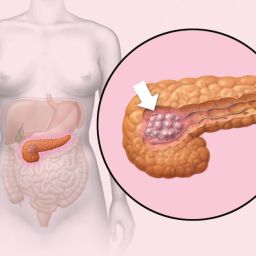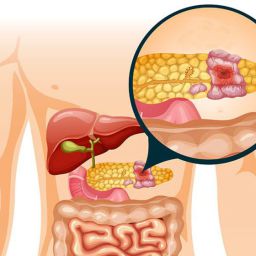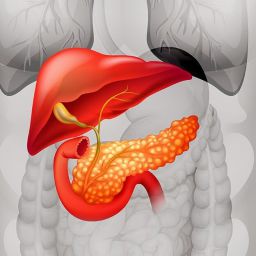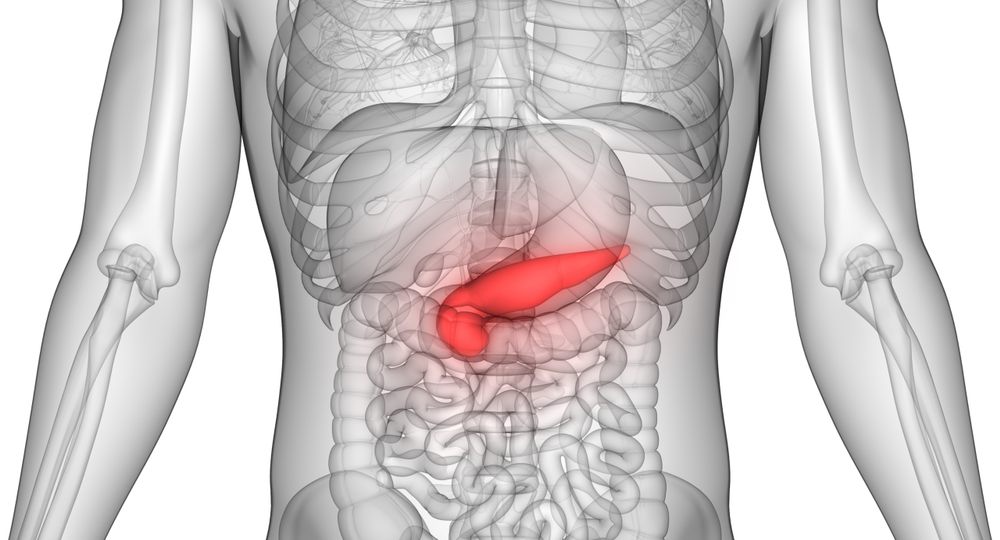
Before diving into the causes, it is important to understand what pancreatic cysts are. Pancreatic cysts are abnormal fluid collections in or around the pancreas. These cysts can vary in size and can be classified into two main categories:
- Non-neoplastic cysts: These are not caused by cancer and generally do not have malignant potential. Examples include pseudocysts and retention cysts.
- Neoplastic cysts: These cysts have the potential to become cancerous. They include types like intraductal papillary mucinous neoplasms (IPMN) and mucinous cystic neoplasms (MCN).
While non-neoplastic cysts are more common, it’s essential to differentiate between the two types because neoplastic cysts may require more intensive management.
Common Causes of Pancreatic Cysts
Pancreatic cysts can develop due to several factors, ranging from chronic pancreatitis to genetic mutations. Below are some of the most common causes:
1. Chronic Pancreatitis
Chronic pancreatitis, an ongoing inflammation of the pancreas, is one of the most significant causes of pancreatic cysts. The inflammation damages the pancreatic tissue, leading to the formation of cysts, which are often called pseudocysts.
- Mechanism: Inflammation can cause ducts to become blocked or obstructed, leading to fluid accumulation. Over time, the accumulated fluid becomes encapsulated, forming a cyst.
- Risk Factors: Alcohol abuse, gallstones, genetic predisposition, and autoimmune conditions are common contributors to chronic pancreatitis.
2. Genetic Mutations
Certain inherited genetic conditions can increase the risk of developing pancreatic cysts. These mutations are often associated with an increased risk of pancreatic cancer.
- Cystic Fibrosis: This is a genetic disorder that affects the pancreas’ ability to produce enzymes. It leads to thickened mucus that can block pancreatic ducts, resulting in cyst formation.
- Hereditary Pancreatitis: Some individuals inherit mutations in genes such as PRSS1 (which encodes a trypsinogen enzyme), making them more likely to develop chronic pancreatitis and pancreatic cysts at an earlier age.
- Von Hippel-Lindau Disease: This rare genetic condition predisposes individuals to develop multiple cysts in various organs, including the pancreas. Pancreatic cysts in these patients are typically neoplastic.
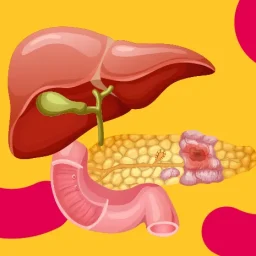
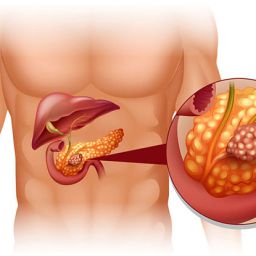
3. Pancreatic Duct Obstruction
Obstruction or blockage of the pancreatic duct can lead to the accumulation of pancreatic juices, which may form cysts. This blockage can occur due to several reasons:
- Gallstones: When gallstones block the bile duct, the pancreatic duct can also become obstructed, leading to cyst formation.
- Tumors: Pancreatic tumors, either benign or malignant, can obstruct the duct, causing fluid to build up and form cysts.
- Trauma or Injury: In rare cases, physical injury to the pancreas, such as from surgery or an accident, can cause a blockage and result in cyst formation.
4. Inflammation or Infection
Acute pancreatitis, which is a sudden inflammation of the pancreas, can also lead to cyst formation, particularly if the inflammation is severe and prolonged.
- Pancreatic Pseudocysts: After an episode of acute pancreatitis, the pancreas may form pseudocysts, which are non-cancerous fluid-filled sacs. These cysts usually contain enzymes, debris, and tissue from the pancreas and do not have a true epithelial lining like other cysts.
- Infection: Sometimes, infections in the pancreas can trigger the formation of cysts as the body attempts to isolate and contain the infection.
5. Age and Gender
As people age, the risk of developing pancreatic cysts increases, particularly non-neoplastic cysts like simple cysts. These cysts are more common in individuals over the age of 60 and may not cause any symptoms.
- Gender Differences: Some studies suggest that men may be more prone to developing pseudocysts related to chronic pancreatitis, while women may be more likely to develop mucinous cysts, which can carry a higher risk of malignancy.
Less Common Causes of Pancreatic Cysts
While the causes mentioned above are the most common, pancreatic cysts can also be caused by a range of rarer conditions and factors.
1. Mucinous Cystic Neoplasms (MCNs)
Mucinous cystic neoplasms are a type of neoplastic cyst that is more common in women and are believed to arise from the ductal epithelium of the pancreas. These cysts have the potential to become malignant over time.
- Causes: MCNs are often linked to genetic mutations and hormonal factors, although the exact cause is not fully understood.
- Risk: If left untreated, MCNs can develop into pancreatic cancer.
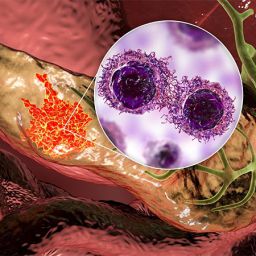
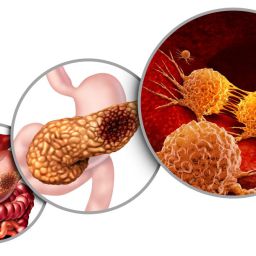
2. Intraductal Papillary Mucinous Neoplasms (IPMNs)
IPMNs are another type of cystic neoplasm that can develop in the pancreatic ducts. These lesions can range from benign to malignant, and they are often associated with a high risk of turning into pancreatic cancer.
- Cause: IPMNs are typically caused by genetic mutations, including mutations in the KRAS gene, which leads to abnormal growth of the pancreatic ducts.
- Risk Factors: Family history of pancreatic cancer, as well as certain inherited genetic conditions, can increase the risk of developing IPMNs.
3. Cystic Lesions Associated with Other Cancers
In some rare cases, pancreatic cysts may be associated with other forms of cancer, such as lymphoma or metastasis from cancers in other organs. These cysts are usually indicative of advanced disease and may require additional diagnostic testing to identify the source of the cancer.
How Are Pancreatic Cysts Diagnosed?
Diagnosing pancreatic cysts involves several imaging techniques, including:
- Ultrasound: Often the first imaging tool used to detect cysts. It is non-invasive and can help identify large cysts.
- CT Scan: A more detailed imaging tool that helps evaluate the size, location, and type of cyst. It is especially helpful in detecting neoplastic cysts.
- MRI and MRCP: Magnetic resonance imaging and magnetic resonance cholangiopancreatography are more advanced techniques used to visualize the pancreatic ducts and surrounding tissue.
- Endoscopic Ultrasound (EUS): A highly sensitive tool for detecting smaller cysts and allowing for tissue sampling if needed.
Treatment and Management
Treatment for pancreatic cysts depends on the type of cyst and whether it is benign or malignant. Some cysts require regular monitoring, while others may require surgical intervention.
- Benign Cysts: Pseudocysts caused by pancreatitis may resolve on their own, but larger or symptomatic cysts may need to be drained or surgically removed.
- Neoplastic Cysts: Mucinous cysts and IPMNs, which have the potential to become cancerous, may require more aggressive treatment, including surgical removal of the cyst or even part of the pancreas.
Pancreatic cysts can develop due to a variety of factors, from chronic inflammation and genetic mutations to pancreatic duct obstruction. While most cysts are benign, some can progress to malignancy, making early detection and monitoring crucial. Understanding the causes and risk factors for pancreatic cyst formation can help individuals and healthcare providers make informed decisions about diagnosis and treatment. If you suspect you have a pancreatic cyst, it’s important to consult with a healthcare professional to determine the appropriate course of action.