Overview of Thyroid Cancer
The thyroid is a butterfly-shaped gland located in the neck, responsible for producing hormones that regulate metabolism, growth, and energy levels. Thyroid cancer occurs when abnormal cells in the thyroid gland begin to grow uncontrollably. There are several types of thyroid cancer, each with its own characteristics and potential for spreading to other parts of the body. The most common types are:
- Papillary Thyroid Cancer (PTC): The most common type of thyroid cancer, accounting for about 70-80% of cases. It is often slow-growing and has a high cure rate. It is more likely to spread to nearby lymph nodes but rarely affects other organs.
- Follicular Thyroid Cancer (FTC): The second most common type, which accounts for about 10-15% of thyroid cancer cases. It can spread to distant parts of the body, especially the lungs and bones.
- Medullary Thyroid Cancer (MTC): A rarer type of thyroid cancer, making up about 4% of all cases. It arises from the C cells of the thyroid and can spread to lymph nodes, liver, and lungs.
- Anaplastic Thyroid Cancer (ATC): A very aggressive and rare form, accounting for about 1-2% of thyroid cancer cases. It has a high tendency to spread quickly to other parts of the body.
Each type of thyroid cancer behaves differently, and understanding the potential for metastasis is important for both treatment planning and prognosis.
Mechanisms of Spread
Thyroid cancer primarily spreads through two main routes: lymphatic spread and hematogenous spread.
Lymphatic Spread

The most common route of metastasis for thyroid cancer is through the lymphatic system. The thyroid gland is surrounded by a network of lymph nodes, which are part of the body’s immune system. These nodes filter lymph fluid and can become a site where cancer cells may collect. Papillary thyroid cancer is particularly known for spreading to regional lymph nodes in the neck.
When thyroid cancer cells enter the lymphatic system, they can travel to nearby lymph nodes and sometimes further to lymph nodes located farther from the thyroid gland. In many cases, the cancer remains confined to these lymph nodes and is not considered a distant spread, which can significantly impact prognosis.
Lymph node metastasis is common in papillary thyroid cancer, but it is also seen in follicular thyroid cancer. However, the presence of lymph node metastasis does not always equate to a worse prognosis, especially if the metastasis is localized and can be treated with surgery or radioactive iodine therapy.
Hematogenous Spread
In addition to lymphatic spread, thyroid cancer can also spread through the bloodstream. This is known as hematogenous metastasis. This type of spread is more common in follicular thyroid cancer and medullary thyroid cancer, though it can also occur in papillary thyroid cancer, albeit less frequently.
When thyroid cancer cells enter the bloodstream, they can travel to distant organs. The most common sites of distant metastasis for thyroid cancer are the lungs and bones. For follicular thyroid cancer, the lungs are the most common site of hematogenous spread, while medullary thyroid cancer tends to metastasize to the liver and lungs.
Anaplastic thyroid cancer, being highly aggressive, has a strong propensity to spread quickly to various organs, including the lungs, liver, bones, and even the brain. Hematogenous spread in anaplastic thyroid cancer is one of the primary reasons this form of thyroid cancer has such a poor prognosis.
Staging and Spread of Thyroid Cancer
The stage of thyroid cancer is an important determinant of its spread. The staging system helps to describe the extent of cancer, from localized growth to more extensive involvement with other parts of the body. The most common staging system for thyroid cancer is the TNM system (Tumor, Node, Metastasis), which considers:

- T (Tumor): The size and extent of the primary tumor in the thyroid.
- N (Node): The involvement of nearby lymph nodes.
- M (Metastasis): Whether cancer has spread to distant parts of the body, such as the lungs or bones.
In early-stage thyroid cancer, particularly in papillary and follicular thyroid cancers, the disease is often localized to the thyroid and may not spread beyond the organ. As the cancer progresses, it can extend to the lymph nodes (regional spread) and even further to distant organs (distant metastasis).
For patients with metastatic thyroid cancer, staging is crucial for determining treatment options and understanding the potential outcomes. Distant metastasis to the lungs, bones, or liver, for instance, may require more aggressive treatment approaches, such as systemic therapies.
Risk Factors for Metastasis
Certain factors increase the likelihood that thyroid cancer will spread. These factors include:
- Cancer Type: As mentioned earlier, papillary thyroid cancer is most likely to spread to regional lymph nodes but rarely to distant sites. Follicular thyroid cancer, on the other hand, is more likely to spread hematogenously to the lungs and bones. Anaplastic thyroid cancer has a high propensity for both local and distant spread.
- Tumor Size: Larger tumors, especially those over 4 cm in diameter, are more likely to metastasize. Smaller tumors tend to stay confined to the thyroid or local lymph nodes.
- Age and Gender: Younger patients, particularly those under 45, tend to have a better prognosis and are less likely to have widespread disease. Thyroid cancer in men tends to be more aggressive and more likely to spread compared to women.
- Genetic Mutations: Certain genetic mutations and syndromes, such as RET proto-oncogene mutations in medullary thyroid cancer or BRAF mutations in papillary thyroid cancer, are associated with more aggressive disease and a higher likelihood of metastasis.
- Histological Subtypes: As mentioned, anaplastic thyroid cancer is highly aggressive and has a propensity to spread early and rapidly. In contrast, the differentiated types (papillary and follicular) have a much lower likelihood of spreading beyond the thyroid, especially when detected early.
Symptoms of Spread
The symptoms of thyroid cancer spread vary depending on the location of the metastasis. Common signs of metastasis include:
- Lung Metastasis: Shortness of breath, persistent cough, chest pain, or coughing up blood can indicate that thyroid cancer has spread to the lungs.
- Bone Metastasis: Bone pain, especially in the spine, ribs, or pelvis, can signal the spread of thyroid cancer to the bones. Fractures or pathological bone changes can occur in advanced stages.
- Liver Metastasis: If thyroid cancer spreads to the liver, patients may experience abdominal pain, jaundice (yellowing of the skin and eyes), unexplained weight loss, or swelling in the abdomen.
- Lymph Node Metastasis: Swelling or enlargement of the lymph nodes in the neck is a common sign of regional spread of thyroid cancer. Sometimes, the nodes may become painful or tender.
Not all patients with metastasis will show symptoms, and some may only be diagnosed with advanced disease after routine imaging tests.
Treatment Options for Metastatic Thyroid Cancer
If thyroid cancer spreads, treatment options will depend on the type of cancer, the extent of the metastasis, and the patient’s overall health. Common treatment strategies for metastatic thyroid cancer include:

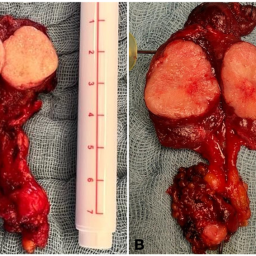
1. Surgery
In many cases, surgery is the first line of treatment for metastatic thyroid cancer. If the cancer has spread to nearby lymph nodes or other accessible areas, surgical removal may be possible. For patients with distant metastases, surgery may be used to remove localized tumors in the lungs or bones, depending on their location and size.
2. Radioactive Iodine Therapy (RAI)
Radioactive iodine (RAI) therapy is particularly effective in treating differentiated thyroid cancers, such as papillary and follicular cancers. After surgery, RAI can help destroy any remaining thyroid tissue or metastasized cancer cells. It works by targeting thyroid cells, including cancer cells, that absorb iodine. This treatment is often used in combination with surgery to ensure the best possible outcome.
3. External Radiation Therapy
In cases where metastasis cannot be treated with surgery or radioactive iodine, external radiation therapy may be used to target and shrink tumors in places like the bones or lungs. This treatment can help manage symptoms and reduce tumor size.
4. Chemotherapy and Targeted Therapy
Chemotherapy is less commonly used for thyroid cancer but may be considered in cases of anaplastic thyroid cancer or medullary thyroid cancer, where other treatments are ineffective. Targeted therapies, such as tyrosine kinase inhibitors (TKIs), are newer options for advanced thyroid cancer and can be effective in targeting specific genetic mutations that drive the cancer.
5. Immunotherapy
In recent years, immunotherapy has emerged as a promising option for treating cancers that have not responded to traditional treatments. While immunotherapy is not yet a standard treatment for thyroid cancer, ongoing clinical trials are evaluating its effectiveness, particularly for aggressive forms of the disease.
Prognosis for Metastatic Thyroid Cancer
The prognosis for metastatic thyroid cancer varies widely based on the type of thyroid cancer, the location of the metastases, and the response to treatment. Differentiated thyroid cancers (papillary and follicular) have a relatively favorable prognosis, even when they metastasize to nearby lymph nodes or distant organs. These cancers often respond well to treatments such as surgery and radioactive iodine therapy.
However, medullary and anaplastic thyroid cancers have a much worse prognosis, particularly when they have spread to distant organs. Anaplastic thyroid cancer, in particular, is considered one of the most aggressive and challenging types to treat, with limited survival rates.
Thyroid cancer can indeed spread, but the likelihood and extent of metastasis depend on the type of cancer, the stage at diagnosis, and various individual factors. While many cases of thyroid cancer are localized and treatable with surgery and radioactive iodine, some forms, especially anaplastic thyroid cancer, can spread aggressively to distant organs, complicating treatment and prognosis.
With early detection and appropriate treatment, thyroid cancer patients have a high survival rate, even in cases where the disease has spread to regional lymph nodes. For patients with advanced or metastatic thyroid cancer, newer treatment options, including targeted therapies and immunotherapy, offer hope for improving outcomes. As always, it is essential for patients to work closely with their healthcare team to determine the best treatment strategy for their specific situation and to monitor the progression of the disease closely.