The Nature of Liver Hemangiomas
Liver hemangiomas are the most common benign liver tumors and are composed of tangled blood vessels. These growths are typically asymptomatic, with most individuals not experiencing any symptoms unless the hemangioma grows large enough to affect surrounding organs. In many cases, liver hemangiomas are found by accident during imaging studies done for other reasons. Although they rarely cause symptoms, they may lead to discomfort or pain if they grow large or exert pressure on surrounding tissues.
Most liver hemangiomas do not require treatment, as they are often small and do not pose significant health risks. In rare instances, large hemangiomas may require medical intervention to prevent complications like bleeding or rupture. However, the vast majority of cases are benign and remain stable over time.
Genetic Factors in Liver Hemangiomas
Despite their benign nature, liver hemangiomas raise an important question: can they be inherited? The current consensus in the medical community is that liver hemangiomas are primarily considered sporadic, meaning they typically arise by chance, without a specific hereditary cause. However, emerging evidence suggests that there may be a genetic predisposition for some individuals, particularly in families with a history of liver hemangiomas.
Liver hemangiomas may not follow clear-cut Mendelian inheritance patterns, where traits are passed down in predictable ways. Instead, their occurrence may be influenced by a combination of genetic factors and environmental triggers. Although the precise genetic mechanisms behind liver hemangiomas are still being studied, there are some indications that family history may increase the likelihood of developing these tumors.
Hereditary Syndromes Linked to Liver Hemangiomas
While most cases of liver hemangiomas appear to be sporadic, there are certain inherited syndromes that may be associated with the development of these tumors. Some genetic conditions predispose individuals to multiple vascular malformations, including hemangiomas in the liver and other organs. Below are a few examples of such syndromes:
1. Klippel-Trenaunay Syndrome (KTS)
Klippel-Trenaunay Syndrome is a rare congenital disorder characterized by abnormal blood vessel formation. Individuals with KTS often develop vascular malformations, such as hemangiomas, in the skin, soft tissues, and internal organs, including the liver. KTS may lead to multiple liver hemangiomas, making it more likely for affected individuals to have a family history of the condition. This syndrome follows an autosomal dominant inheritance pattern, meaning that a person with KTS has a 50% chance of passing the disorder to their offspring.
2. Sturge-Weber Syndrome
Sturge-Weber Syndrome is another rare genetic disorder that involves abnormal blood vessel growth, often affecting the skin, eyes, and brain. It is possible for individuals with Sturge-Weber Syndrome to also develop liver hemangiomas, although this is not a common feature of the condition. Sturge-Weber Syndrome is also associated with neurological and vascular abnormalities, and like Klippel-Trenaunay Syndrome, it may be inherited in an autosomal dominant manner.
3. Hereditary Hemorrhagic Telangiectasia (HHT)
Hereditary Hemorrhagic Telangiectasia, also known as Osler-Weber-Rendu syndrome, is a genetic disorder that causes abnormal blood vessel formation. While it primarily affects the skin and mucous membranes, it can also lead to vascular malformations in internal organs, including the liver. In some cases, individuals with HHT may develop liver hemangiomas as a secondary manifestation of the condition. HHT is inherited in an autosomal dominant manner, meaning that each child of an affected individual has a 50% chance of inheriting the condition.
Is There a Likelihood of Liver Hemangiomas Occurring in Family Members?

Although liver hemangiomas are most often sporadic, there is a possibility that family members may develop them as well. Research on the genetic factors behind liver hemangiomas is still limited, but some studies suggest that a family history of liver hemangiomas can increase the likelihood of developing them. For instance, families with a history of these benign liver tumors may notice patterns of hemangiomas in multiple relatives, although the risk remains relatively low for most people.
In general, liver hemangiomas do not exhibit the same clear inheritance patterns as some other genetic disorders. The increased occurrence in family members may be the result of shared genetic predispositions or environmental factors that influence the development of these tumors. Additionally, certain genetic syndromes, like those mentioned above, can increase the likelihood of developing liver hemangiomas across multiple generations.
It is important to note that in most cases, liver hemangiomas are isolated incidents in a person’s medical history, with no other family members being affected. However, individuals with a family history of liver hemangiomas should be vigilant about their health and consider discussing any concerns with their healthcare provider.
Genetic Testing and Screening for Liver Hemangiomas
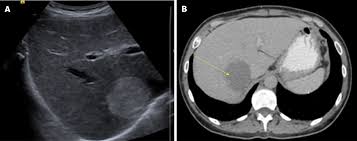
Given that liver hemangiomas are most often asymptomatic and benign, routine genetic testing for the condition is not generally recommended. However, individuals with a known family history of liver hemangiomas or related genetic conditions, such as Klippel-Trenaunay Syndrome or Hereditary Hemorrhagic Telangiectasia, may benefit from screening to detect the presence of hemangiomas in the liver and other organs.
For those with a genetic predisposition to multiple liver hemangiomas, early detection and regular monitoring can help ensure that any potential complications are identified promptly. Imaging tests, such as ultrasounds, CT scans, or MRIs, can be used to detect liver hemangiomas and assess their size and growth over time.
Risk Factors for Developing Liver Hemangiomas
In addition to family history, several factors may influence the likelihood of developing liver hemangiomas. These risk factors include:
- Gender: Liver hemangiomas are more common in women, particularly during childbearing years. This suggests that hormonal factors may play a role in their development.
- Hormonal Influences: There is evidence to suggest that hormones, particularly estrogen, may contribute to the growth of liver hemangiomas. Women who have been pregnant or are taking hormone replacement therapy may be at a higher risk.
- Age: Liver hemangiomas are most often diagnosed in adults, typically in their 30s or 40s. Although they can occur in children, the vast majority of cases are found in adults.
- Obesity: While obesity is not directly linked to the development of liver hemangiomas, individuals with obesity may be at an increased risk of developing other liver-related conditions, such as fatty liver disease, which may co-occur with hemangiomas.
Managing Liver Hemangiomas in Families with a History
For individuals with a family history of liver hemangiomas, maintaining good liver health is essential. While the majority of liver hemangiomas do not require treatment, monitoring liver function and undergoing regular imaging tests can help detect any changes in the size or number of hemangiomas.
Adopting a healthy lifestyle, including a balanced diet, regular exercise, and avoiding excessive alcohol consumption, can also contribute to overall liver health. People with a family history of liver hemangiomas should discuss their concerns with a healthcare provider to determine the best approach to monitoring their liver health.
Liver hemangiomas, while typically benign and asymptomatic, can raise important questions about their causes and whether they may be inherited. In most cases, liver hemangiomas are sporadic and not inherited in a straightforward genetic pattern. However, certain genetic syndromes, such as Klippel-Trenaunay Syndrome, Sturge-Weber Syndrome, and Hereditary Hemorrhagic Telangiectasia, are linked to the development of these tumors, and there may be an increased risk of occurrence in family members for individuals with these conditions.
Though the inheritance of liver hemangiomas is not fully understood, families with a history of the condition may have a slightly higher risk of developing liver hemangiomas. Regular screening and monitoring are recommended for those with a known family history or other risk factors. In most cases, liver hemangiomas do not pose a significant threat to health, but they should be carefully managed and monitored for any potential complications.