1. Genetic Factors and Cancer Metastasis
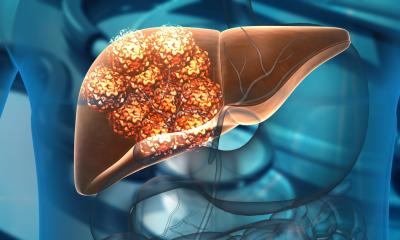
Genetic mutations in tumor cells drive the processes of cancer initiation, growth, and spread. Metastasis is a complex and multistep process that involves genetic and epigenetic changes within cancer cells. These changes enable the tumor cells to invade surrounding tissues, enter the bloodstream or lymphatic system, and migrate to distant organs such as the liver. The question arises: do genetic factors play a direct role in determining whether a cancer will metastasize to the liver?
1.1 Oncogenes and Tumor Suppressors in Metastasis
Certain genes that regulate cell growth and division are critical in determining the aggressiveness of a cancer. These include oncogenes (genes that, when mutated, promote cancerous growth) and tumor suppressor genes (genes that normally act to prevent tumor formation). Mutations in these genes can influence the likelihood of metastasis to the liver.
Oncogenes such as RAS, HER2, and MYC are frequently found to be overactive in many cancers that metastasize to the liver, including colorectal cancer, breast cancer, and lung cancer. These mutations promote uncontrolled cell growth, enabling cancer cells to invade neighboring tissues and enter the bloodstream or lymphatic system.
Similarly, tumor suppressor genes like TP53 (which is commonly mutated in liver cancer and other cancers) are involved in the regulation of cell death and DNA repair. When these genes are altered, cancer cells may accumulate more mutations, making them more likely to spread and colonize distant organs, including the liver.
1.2 The Role of Genetic Heterogeneity
Genetic heterogeneity, which refers to the genetic diversity within a tumor, can influence metastatic potential. Tumors are composed of multiple subclones of cancer cells, each of which may have different genetic characteristics. Some of these subclones may possess genetic mutations that enable them to invade tissues more effectively, migrate to the liver, and survive in the hostile microenvironment of a metastatic site.
The genetic diversity of tumors can vary significantly from one patient to another, and this heterogeneity can dictate the ability of cancer cells to adapt to different organs, including the liver. Moreover, genetic changes that enable tumor cells to evade the immune system or resist chemotherapy may also increase the likelihood of liver metastasis and further spread.
2. Genetic Predisposition to Liver Metastasis
While most genetic mutations associated with liver metastasis are acquired (somatic mutations), some patients may have a genetic predisposition that increases their likelihood of developing liver metastases. These inherited genetic factors may influence various aspects of cancer progression, including the ability of cancer cells to metastasize to the liver.
2.1 Hereditary Cancer Syndromes
Certain hereditary cancer syndromes increase the risk of both primary liver cancer and metastasis to the liver. For instance, familial adenomatous polyposis (FAP), which is caused by mutations in the APC gene, increases the risk of colorectal cancer, a common origin for liver metastasis. Patients with FAP may have an increased likelihood of developing liver metastases if their colorectal cancer spreads.
Other genetic conditions, such as hereditary breast and ovarian cancer syndrome, caused by mutations in the BRCA1 and BRCA2 genes, may also predispose individuals to aggressive forms of breast cancer that have a higher chance of metastasizing to the liver. Furthermore, mutations in genes involved in DNA repair mechanisms, like MLH1 and MSH2, which are implicated in Lynch syndrome, have been associated with an increased risk of colorectal cancer and its metastasis to the liver.
2.2 Host Genetic Factors and Liver Microenvironment
In addition to genetic mutations in tumor cells, genetic factors that influence the liver’s microenvironment can also affect the likelihood of metastasis. The liver is composed of various cell types, including hepatocytes, endothelial cells, and immune cells, all of which contribute to the organ’s function and response to cancer.
Certain genetic variations in liver cells can make the liver more susceptible to the growth and survival of metastatic cancer cells. For example, polymorphisms in genes that regulate immune responses, such as TLR4 (Toll-like receptor 4), may influence the liver’s ability to mount an immune response against cancer cells. Additionally, variations in genes involved in liver metabolism and detoxification may help cancer cells adapt to the liver environment and establish metastatic lesions.
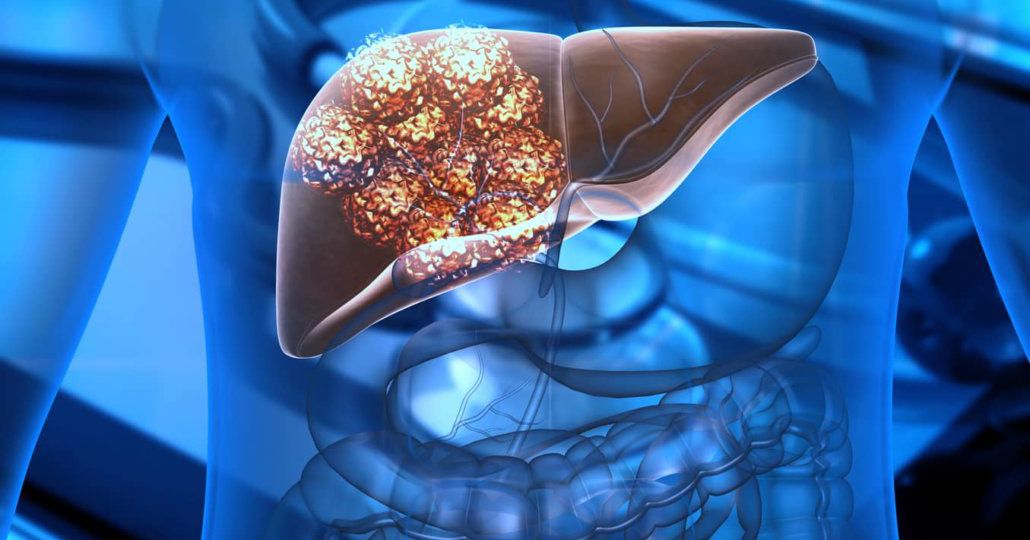
3. Molecular Mechanisms of Liver Metastasis
The ability of cancer cells to spread to the liver and other distant organs involves a series of complex molecular mechanisms, which are influenced by genetic factors.
3.1 Epithelial-to-Mesenchymal Transition (EMT)
Epithelial-to-mesenchymal transition (EMT) is a process by which epithelial cancer cells lose their adhesive properties and gain the ability to migrate and invade other tissues. Genetic alterations that promote EMT are associated with a higher likelihood of metastasis. For example, mutations in E-cadherin and β-catenin, which are involved in cell-cell adhesion, are often found in cancers that spread to the liver.
During EMT, cancer cells acquire a more migratory phenotype, which facilitates their movement through the bloodstream to distant organs like the liver. These changes are often regulated by oncogenes such as SNAIL, TWIST, and ZEB1, which are activated by genetic mutations or epigenetic changes.
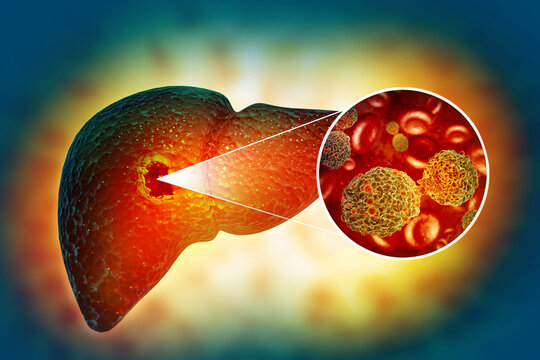
3.2 Angiogenesis and Vascular Invasion
For metastasis to occur, cancer cells must also be able to establish a blood supply at the metastatic site. Angiogenesis, the formation of new blood vessels, is essential for the growth and survival of metastatic tumors. Genetic mutations in genes like VEGF (vascular endothelial growth factor) can promote angiogenesis and help metastatic cancer cells survive in the liver.
Additionally, the ability of cancer cells to invade blood vessels (vascular invasion) is critical for metastasis. Mutations in genes that regulate the cytoskeleton, such as RHOA, enable cancer cells to invade blood vessels and spread through the circulatory system to organs like the liver.
4. Genetic Testing and Personalized Medicine for Liver Metastasis
Understanding the genetic factors involved in liver metastasis has profound implications for diagnosis, treatment, and patient outcomes. Advances in genetic testing allow oncologists to identify specific genetic mutations that may increase the risk of metastasis, enabling personalized treatment approaches.
4.1 Targeted Therapies
Targeted therapies that specifically address genetic mutations involved in metastasis are an area of active research. For example, drugs targeting the RAS pathway are being investigated for colorectal cancer, which frequently metastasizes to the liver. Similarly, HER2 inhibitors are used for breast cancer patients with liver metastasis who overexpress the HER2 protein.
By identifying genetic alterations in tumors, oncologists can select targeted therapies that are more likely to be effective against specific cancer types and genetic profiles, improving the chances of controlling liver metastasis and preventing further spread.
4.2 Immunotherapy
Immunotherapy, which works by stimulating the body’s immune system to recognize and attack cancer cells, has shown promise in treating metastatic cancers. Genetic testing can help identify patients who are more likely to benefit from immunotherapy, particularly those whose tumors have specific genetic characteristics, such as PD-L1 expression or MSI-H status, which are often found in tumors that metastasize to the liver.
Genetic factors play a crucial role in liver metastasis, influencing both the ability of cancer cells to spread and the environment of the liver itself. While many of the mutations driving liver metastasis are acquired, there are also inherited genetic predispositions that increase the risk of liver involvement. Understanding these genetic factors is essential for developing more effective treatments, improving early detection, and personalizing therapy for patients with liver metastases. With ongoing advances in genetic research and personalized medicine, the future of liver metastasis management looks promising, offering hope for improved outcomes and survival for patients affected by this challenging condition.