1. The Role of the Immune System in Anal Fistula Formation
The formation and persistence of an anal fistula are closely linked to the body’s immune system response. Normally, the immune system is tasked with protecting the body from infections, healing injuries, and managing inflammation. However, in the case of anal fistulas, the immune system’s reaction to the infection or injury within the anal glands can sometimes go awry, leading to chronic inflammation, the formation of abscesses, and the subsequent development of fistulas.
Inflammation and Immune Response

The immune response plays a critical role in the development of anal fistulas. When an infection occurs in the anal glands, the body’s immune system sends white blood cells and inflammatory mediators to the affected area to combat the infection. This inflammation is intended to help the body heal. However, if the infection persists or if the immune system is unable to clear it completely, the immune response can lead to the formation of a fistula.
The inflammatory process may cause tissue damage, and instead of promoting healing, it can lead to the chronic drainage seen in anal fistulas. Inflammatory bowel diseases (IBD), such as Crohn’s disease, are a prime example of conditions that affect the immune system and predispose individuals to develop anal fistulas. Chronic inflammation in the digestive tract, particularly in the rectum and anus, weakens the tissues and leads to the formation of fistulas.
The Role of the Microbiome
The gut microbiome—the diverse community of bacteria living in the intestines—also plays a significant role in the immune system’s function. In a healthy individual, the gut microbiome helps regulate the immune system, promoting appropriate responses to infection while preventing excessive inflammation. However, an imbalance in the microbiome, known as dysbiosis, can contribute to immune system dysfunction.
In individuals with conditions like Crohn’s disease or ulcerative colitis, which are characterized by chronic inflammation and immune dysregulation, dysbiosis is common. This imbalance in the microbiome may exacerbate inflammation in the anal area and contribute to the formation and persistence of anal fistulas.
2. Impact of Anal Fistulas on the Immune System
While anal fistulas are primarily localized to the anal area, they can have broader implications for the immune system. The chronic nature of the condition, along with the repeated infections and inflammation, can strain the body’s immune system in several ways.
Chronic Inflammation and Immune Fatigue
The prolonged inflammation caused by an anal fistula can contribute to immune system fatigue. Inflammation is a necessary part of the immune response, but when it becomes chronic, the immune system may become overtaxed. Chronic inflammation in the anal region can lead to a cycle of ongoing infection and healing that challenges the body’s ability to regulate immune function effectively.
In addition, some of the treatments used to manage anal fistulas, such as immunosuppressive medications for conditions like Crohn’s disease, can further impair immune function. These medications reduce the body’s ability to fight infections and may leave individuals more vulnerable to secondary infections or complications.
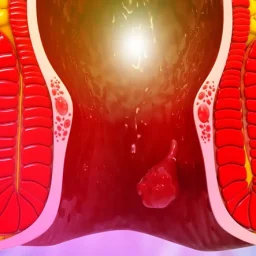
Risk of Systemic Infections
Though anal fistulas are localized to the anal area, their presence can increase the risk of systemic infections. The chronic discharge from the fistula, which often contains bacteria, can spread to surrounding tissues, increasing the likelihood of secondary infections. In severe cases, the infection may even enter the bloodstream, leading to sepsis, a life-threatening condition.
For individuals with already compromised immune systems, such as those with HIV/AIDS or autoimmune disorders, the risk of these systemic infections is even greater. Managing an anal fistula in such patients requires careful monitoring and may involve additional treatments to support immune function.
Worsening of Underlying Conditions
In some cases, the presence of an anal fistula can worsen underlying conditions that impact immune function. For instance, individuals with Crohn’s disease, which causes chronic inflammation in the gastrointestinal tract, are more likely to experience anal fistulas. The continuous inflammation in the digestive tract and the anal region can perpetuate immune system dysfunction, making it harder for the body to heal and maintain proper immune responses.
3. Anal Fistulas in Immunocompromised Individuals
The relationship between anal fistulas and the immune system becomes even more complex when individuals are immunocompromised. People with weakened immune systems, whether due to conditions like HIV, cancer treatment, or the use of immunosuppressive drugs for autoimmune diseases, face unique challenges when dealing with anal fistulas.
Impact of Immunosuppressive Medications
Immunosuppressive medications, such as corticosteroids or biologics, are commonly used to manage conditions like Crohn’s disease, ulcerative colitis, or other autoimmune disorders. These medications can help reduce inflammation but at the cost of weakening the immune system. As a result, individuals on immunosuppressive drugs may be more susceptible to infections and may experience delayed healing of anal fistulas.
Additionally, the use of these medications can alter the body’s ability to produce an effective immune response, potentially allowing infections to persist longer and further complicating the healing process of an anal fistula.
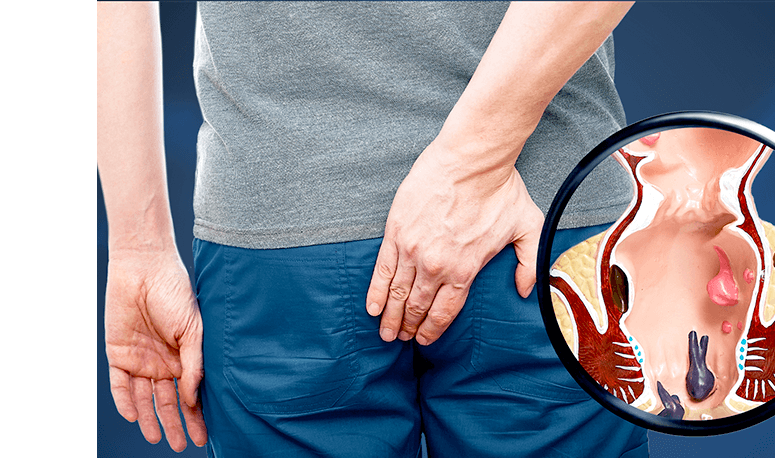
Complications in Immunocompromised Patients
Immunocompromised individuals who develop anal fistulas may face a higher risk of complications. In addition to the chronic inflammation and infection that is characteristic of anal fistulas, these patients may be more likely to experience severe infections, poor wound healing, and an increased risk of developing fistulas in multiple areas. Moreover, the risk of developing abscesses and the spread of infection to nearby tissues or organs is heightened.
In these cases, it is crucial for healthcare providers to adopt a comprehensive treatment plan that addresses both the fistula and the underlying immunosuppressed condition.
4. Treatment Approaches for Anal Fistulas and Immune System Support
Treating an anal fistula involves addressing both the physical symptoms and the underlying immune response. Various medical and surgical treatments are available, depending on the severity and location of the fistula, as well as the patient’s overall health and immune status.
Antibiotics and Anti-inflammatory Medications
Antibiotics are often prescribed to control infections associated with anal fistulas. In cases where the patient has an underlying inflammatory condition such as Crohn’s disease, anti-inflammatory medications may also be used to reduce the immune system’s inflammatory response. These drugs help limit the damage caused by the immune system’s overreaction and promote healing.
However, the use of antibiotics and anti-inflammatory medications should be carefully managed to avoid further compromising the immune system.
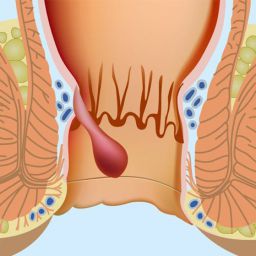
Surgical Intervention
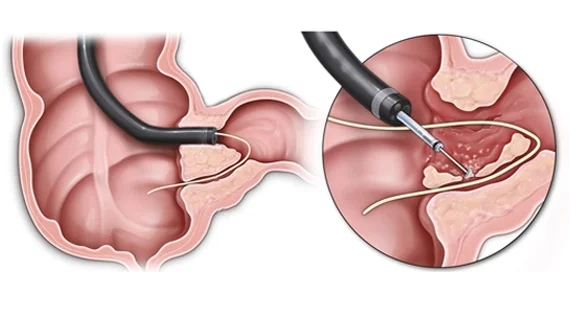
In many cases, surgical treatment is required to close or repair the fistula. Surgical procedures may include fistulotomy (cutting open the fistula to allow it to heal), seton placement (a surgical thread placed through the fistula to help drain infection), or flap procedures (where tissue is used to close the fistula). The choice of surgery depends on the type and location of the fistula, as well as the overall health of the patient.
For individuals with compromised immune systems, surgery may need to be postponed until the infection is under control and the immune system is better able to support the healing process. In some cases, a multidisciplinary team of specialists, including immunologists, gastroenterologists, and surgeons, may be involved in the treatment plan.
Supportive Care for Immunocompromised Patients
For immunocompromised individuals, treatment must focus not only on the fistula itself but also on supporting the immune system. This can include the use of medications to bolster immune function, lifestyle changes to improve overall health, and close monitoring for infections.
Regular follow-up care is crucial to ensure that any complications, such as infection or delayed healing, are promptly addressed. Patients should be educated on proper hygiene and wound care to prevent further infection and ensure optimal healing conditions.
Anal fistulas are a challenging and often painful condition, and their impact on the immune system adds another layer of complexity to their management. The chronic inflammation and infection that characterize anal fistulas can strain the body’s immune system, particularly in individuals with underlying conditions that compromise immunity. A comprehensive treatment approach, which includes managing both the fistula and the immune response, is essential for effective healing and recovery.